NAPLEX
The questions in this section are intended to test your knowledge and skills in pharmacy practice including pharmacy calcuations and biostatistics for pharmacy student pursuing to get license. Select all that applies. May have multiple answers. ( Keep in mind the calulation questions on the NAPLEX exam are NOT multiple choice, you are required to type in your answers)
Click on the right arrow to go to the next question. If the arrow is missing hover your mouse to the lower right, above the ad until the mouse is clickable.
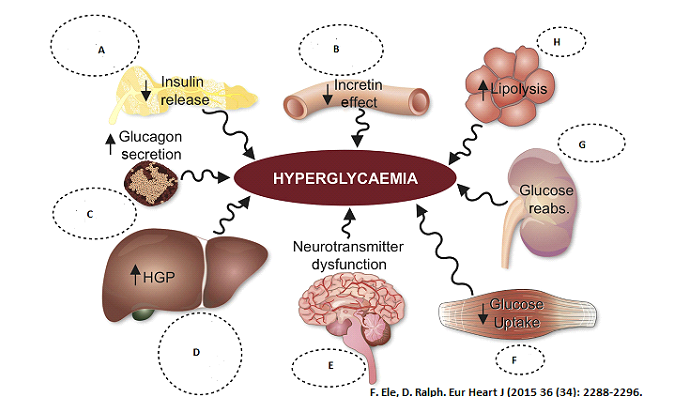 Select the class of Anti-diabetic medication that works in the specified organ to prevent hyperglycemia. Select all that applies.
Pancreases (A)
Select the class of Anti-diabetic medication that works in the specified organ to prevent hyperglycemia. Select all that applies.
Pancreases (A)
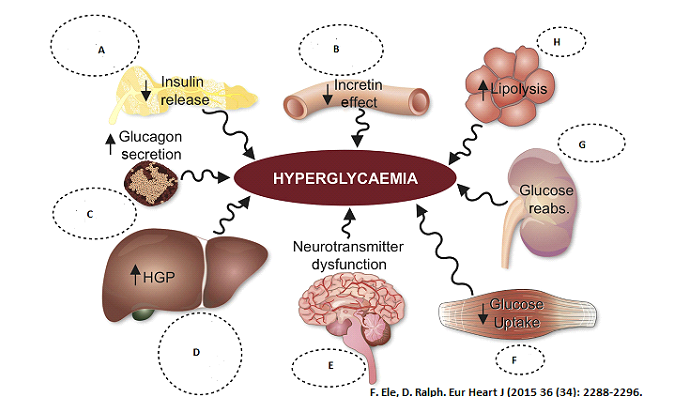 Select the class of Anti-diabetic medication that works in the specified organ to prevent hyperglycemia. Select all that applies.
GI tract (B)
Select the class of Anti-diabetic medication that works in the specified organ to prevent hyperglycemia. Select all that applies.
GI tract (B)
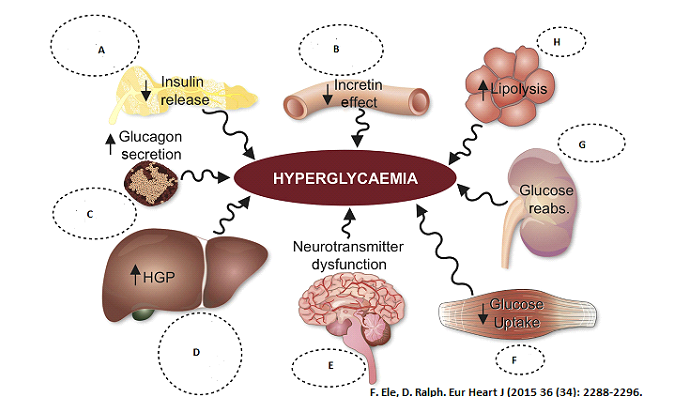 Select the class of Anti-diabetic medication that works in the specified organ to prevent hyperglycemia. Select all that applies.
Alpha cells in pancreases
Select the class of Anti-diabetic medication that works in the specified organ to prevent hyperglycemia. Select all that applies.
Alpha cells in pancreases
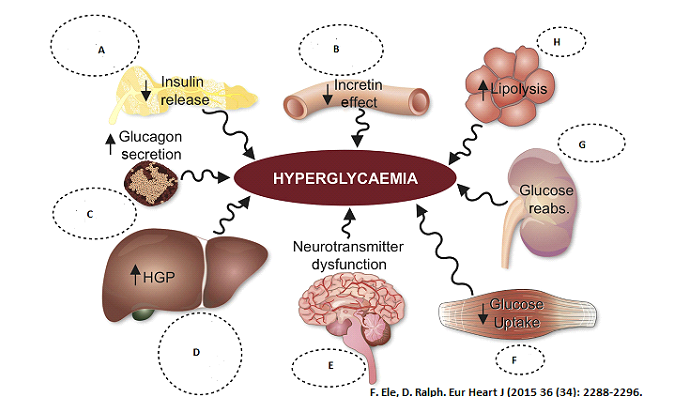 Select the class of Anti-diabetic medication that works in the specified organ to prevent hyperglycemia. Select all that applies.
Liver (D)
Select the class of Anti-diabetic medication that works in the specified organ to prevent hyperglycemia. Select all that applies.
Liver (D)
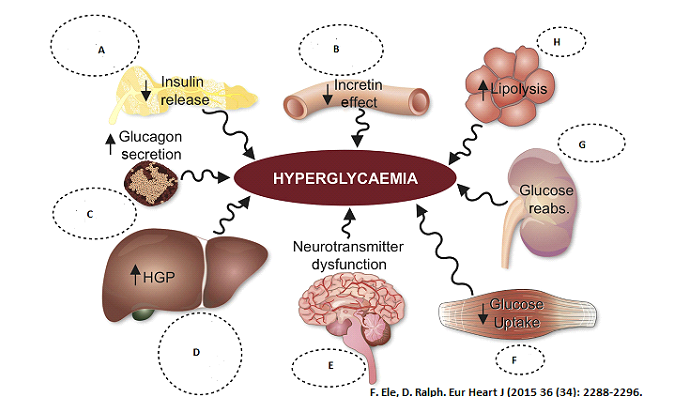 Select the class of Anti-diabetic medication that works in the specified organ to prevent hyperglycemia. Select all that applies.
Brain (E)
Select the class of Anti-diabetic medication that works in the specified organ to prevent hyperglycemia. Select all that applies.
Brain (E)
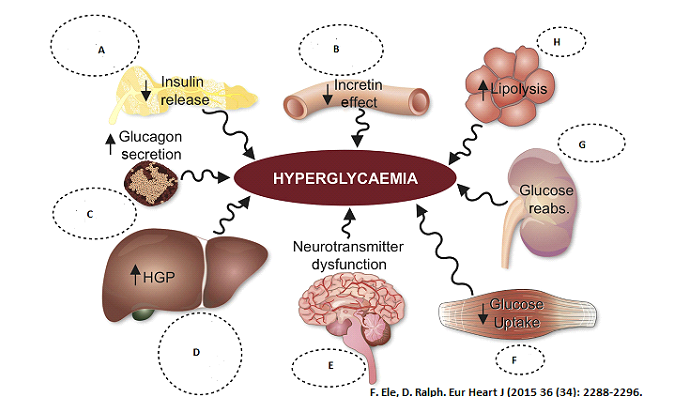 Select the class of Anti-diabetic medication that works in the specified organ to prevent hyperglycemia. Select all that applies.
Muscle (F)
Select the class of Anti-diabetic medication that works in the specified organ to prevent hyperglycemia. Select all that applies.
Muscle (F)
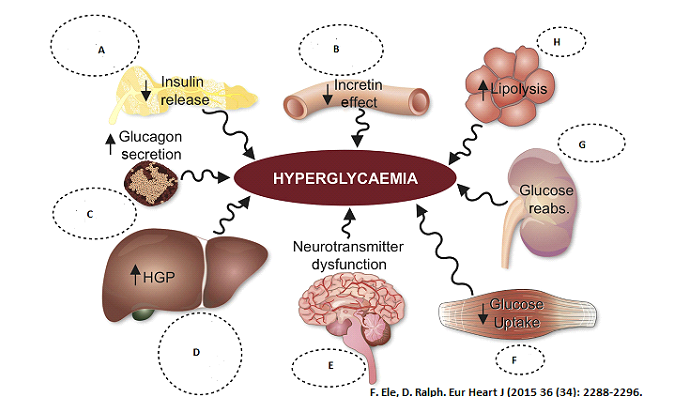 Select the class of Anti-diabetic medication that works in the specified organ to prevent hyperglycemia. Select all that applies.
Kidney (G)
Select the class of Anti-diabetic medication that works in the specified organ to prevent hyperglycemia. Select all that applies.
Kidney (G)
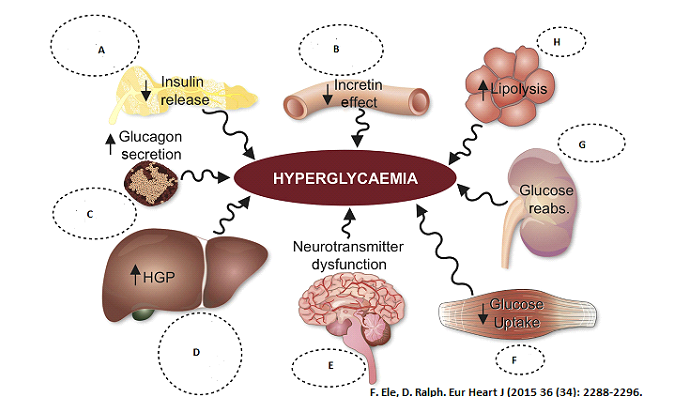 Select the class of Anti-diabetic medication that works in the specified organto prevent hyperglycemia. Select all that applies.
Fat Tissue (H)
Select the class of Anti-diabetic medication that works in the specified organto prevent hyperglycemia. Select all that applies.
Fat Tissue (H)
NAPLEX Practice Questions
Congratulations - you have completed NAPLEX Practice Questions.
You scored %%SCORE%% out of %%TOTAL%%.
Your performance has been rated as %%RATING%%
Your answers are highlighted below.
Question 1 |
LN is 84 YOM who is in hospital for a back surgery.His height is 5 feet and 4 inches, weight 85 kg and NKDA. His past medical history includes hypertension, diabetes mellitus, major depression, hypothyroidism and chronic back pain. Post-op day 1, LN’s medication includes Dexamethasone 8mg iv q6h with taper dosing, Ondansetron 4mg iv q6h prn for N/V, Levothyroxine 0.075mg po daily, Lisinopril 10mg po daily, Citalopram 20mg po daily, Docusate sodium / Senna 1 tab po twice a day, Bisacodyl 10mg suppository daily prn for constipation, Famotidine 20mg iv q12hr, Metoclopramide 10mg iv q6h, Metformin 500mg po bid, D51/2NS with 20K at 125mls/hour and Hydromorphone PCA at 0.2mg/hour of basal rate, demand dose 0.1mg. lock-out every 6min, one hour limit 2.2mg/hour. Pertinent morning labs includes serum creatinine 1.4mg/dl, Mg 1.5mg/dl, K 5.0mmol/L, Na 135mmol/L.
Which of the following medication may increase LN’s Blood glucose?
Lisinopril | |
Dexamethasone | |
Famotidine | |
Metoclopramide | |
Hydromorphone |
Question 1 Explanation:
Dexamethasone can increase LN’s blood glucose. All glucocorticosteroids are known to increase blood glucose. Blood glucose would need to be monitored while LN is being treated with dexamethasone.
Reference:
Inzucchi S, Bergenstal R, Buse J, et al. Management of hyperglycemia in type 2 diabetes: a patient- centered approach. Diabetes Care 2012;35:1364-79.
Reference:
Inzucchi S, Bergenstal R, Buse J, et al. Management of hyperglycemia in type 2 diabetes: a patient- centered approach. Diabetes Care 2012;35:1364-79.
Question 2 |
LN is 84 YOM who is in hospital for a back surgery.His height is 5 feet and 4 inches, weight 85 kg and NKDA. His past medical history includes hypertension, diabetes mellitus, major depression, hypothyroidism and chronic back pain. Post-op day 1, LN’s medication includes Dexamethasone 8mg iv q6h with taper dosing, Ondansetron 4mg iv q6h prn for N/V, Levothyroxine 0.075mg po daily, Lisinopril 10mg po daily, Citalopram 20mg po daily, Docusate sodium / Senna 1 tab po twice a day, Bisacodyl 10mg suppository daily prn for constipation, Famotidine 20mg iv q12hr, Metoclopramide 10mg iv q6h, Metformin 500mg po bid, D51/2NS with 20K at 125mls/hour and Hydromorphone PCA at 0.2mg/hour of basal rate, demand dose 0.1mg. lock-out every 6min, one hour limit 2.2mg/hour. Pertinent morning labs includes serum creatinine 1.4mg/dl, Mg 1.5mg/dl, K 5.0mmol/L, Na 135mmol/L.
Which of the following medication may cause tardive dyskinesia when given at a higher dose and for a long duration?
Lisinopril | |
Dexamethasone | |
Famotidine | |
Metoclopramide | |
Hydromorphone |
Question 2 Explanation:
Metoclopramide may cause tardive dyskinesia when given at a higher dose and for a long duration of time of more than 3 months. Tardive dyskinesia is also listed as a Boxed Warning for metoclopramide. Tardive dyskinesia is a serious movement disorder that is irreversible. The risk increases with duration of treatment and the total cumulative dose. If signs or symptoms of tardive dyskinesia develop, then metoclopramide should be discontinued. There is currently no known treatment for it, but symptoms can lessen or resolve after metoclopramide is stopped. Treatment should not be more than 12 weeks unless the benefits outweigh the risks of developing tardive dyskinesia.
Reference:
Metoclopramide hydrochloride tablet package insert. Rockford, IL: Mylan Institutional Inc.; 2016 Oct.
Reference:
Metoclopramide hydrochloride tablet package insert. Rockford, IL: Mylan Institutional Inc.; 2016 Oct.
Question 3 |
LN is 84 YOM who is in hospital for a back surgery.His height is 5 feet and 4 inches, weight 85 kg and NKDA. His past medical history includes hypertension, diabetes mellitus, major depression, hypothyroidism and chronic back pain. Post-op day 1, LN’s medication includes Dexamethasone 8mg iv q6h with taper dosing, Ondansetron 4mg iv q6h prn for N/V, Levothyroxine 0.075mg po daily, Lisinopril 10mg po daily, Citalopram 20mg po daily, Docusate sodium / Senna 1 tab po twice a day, Bisacodyl 10mg suppository daily prn for constipation, Famotidine 20mg iv q12hr, Metoclopramide 10mg iv q6h, Metformin 500mg po bid, D51/2NS with 20K at 125mls/hour and Hydromorphone PCA at 0.2mg/hour of basal rate, demand dose 0.1mg. lock-out every 6min, one hour limit 2.2mg/hour. Pertinent morning labs includes serum creatinine 1.4mg/dl, Mg 1.5mg/dl, K 5.0mmol/L, Na 135mmol/L.
Which of the following medication may cause psychotic episode such as emotional lability, hallucinations, mania, mood swings and schizophrenic reasons?
Lisinopril | |
Dexamethasone | |
Famotidine | |
Metoclopramide | |
Hydromorphone |
Question 3 Explanation:
Dexamethasone is associated with psychiatric disturbances. Corticosteroids may exacerbate pre-existing psychiatric conditions.
Reference:
Cerullo MA, Corticosteroid-induced mania: Prepare for the unpredictable, Current Psychiatry. 2006 June;5(6):43-50.
Reference:
Cerullo MA, Corticosteroid-induced mania: Prepare for the unpredictable, Current Psychiatry. 2006 June;5(6):43-50.
Question 4 |
LN is 84 YOM who is in hospital for a back surgery.His height is 5 feet and 4 inches, weight 85 kg and NKDA. His past medical history includes hypertension, diabetes mellitus, major depression, hypothyroidism and chronic back pain. Post-op day 1, LN’s medication includes Dexamethasone 8mg iv q6h with taper dosing, Ondansetron 4mg iv q6h prn for N/V, Levothyroxine 0.075mg po daily, Lisinopril 10mg po daily, Citalopram 20mg po daily, Docusate sodium / Senna 1 tab po twice a day, Bisacodyl 10mg suppository daily prn for constipation, Famotidine 20mg iv q12hr, Metoclopramide 10mg iv q6h, Metformin 500mg po bid, D51/2NS with 20K at 125mls/hour and Hydromorphone PCA at 0.2mg/hour of basal rate, demand dose 0.1mg. lock-out every 6min, one hour limit 2.2mg/hour. Pertinent morning labs includes serum creatinine 1.4mg/dl, Mg 1.5mg/dl, K 5.0mmol/L, Na 135mmol/L.
Which of the following medication may significantly cause QT prolongation?
Lisinopril | |
Levothyroxine | |
Metformin | |
Hydromorphone | |
Citalopram |
Question 4 Explanation:
Celexa causes dose-dependent QT interval prolongation, which can cause Torsades de Pointes, ventricular tachycardia, and sudden death. Celexa is not recommended for use at doses greater than 40 mg per day because such doses cause too large an effect on the QT interval and confer no additional benefit. Celexa should be discontinued in patients found to have persistent QTc measurements greater than 500 ms.Ondansetron and Famotidine may cause QT prolongation. Ondansetron may cause QT prolongation. However, this would be dose-dependent. Doses greater than 16 mg of Ondansetron IV are no longer recommended due to an increased risk of QT prolongation. Famotidine may prolong the QT interval; this has been reported in those with renal dysfunction. There have also been reports of torsade de pointes. Use of all three medications may result in an arrhythmia occurring since both have the potential to prolong the QT interval. Therefore, close monitoring is recommended or discontinuation of one medication. The other medications listed do not have this warning/precaution.
Reference:
I. FDA Drug Safety Communication: Revised recommendations for Celexa (citalopram hydrobromide) related to a potential risk of abnormal heart rhythms with high doses. Available at: http://www.fda.gov/Drugs/DrugSafety/ucm297391.htm Accessed January 17, 2017.
II. Nachimuthu S, Assar MD, et al. Drug-induced QT interval prolongation: mechanisms and clinical management. Ther Adv Drug Saf. 2012 Oct; 3(5): 241–253. doi: 10.1177/2042098612454283. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4110870
Reference:
I. FDA Drug Safety Communication: Revised recommendations for Celexa (citalopram hydrobromide) related to a potential risk of abnormal heart rhythms with high doses. Available at: http://www.fda.gov/Drugs/DrugSafety/ucm297391.htm Accessed January 17, 2017.
II. Nachimuthu S, Assar MD, et al. Drug-induced QT interval prolongation: mechanisms and clinical management. Ther Adv Drug Saf. 2012 Oct; 3(5): 241–253. doi: 10.1177/2042098612454283. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4110870
Question 5 |
LN is 84 YOM who is in hospital for a back surgery.His height is 5 feet and 4 inches, weight 85 kg and NKDA. His past medical history includes hypertension, diabetes mellitus, major depression, hypothyroidism and chronic back pain. Post-op day 1, LN’s medication includes Dexamethasone 8mg iv q6h with taper dosing, Ondansetron 4mg iv q6h prn for N/V, Levothyroxine 0.075mg po daily, Lisinopril 10mg po daily, Citalopram 20mg po daily, Docusate sodium / Senna 1 tab po twice a day, Bisacodyl 10mg suppository daily prn for constipation, Famotidine 20mg iv q12hr, Metoclopramide 10mg iv q6h, Metformin 500mg po bid, D51/2NS with 20K at 125mls/hour and Hydromorphone PCA at 0.2mg/hour of basal rate, demand dose 0.1mg. lock-out every 6min, one hour limit 2.2mg/hour. Pertinent morning labs includes serum creatinine 1.4mg/dl, Mg 1.5mg/dl, K 5.0mmol/L, Na 135mmol/L.
Which of the following medication/s should LN be on to prevent the most common side effect of hydromorphone?
Ondansetron for N/V | |
Dexamethasone for N/V | |
Insulin Sliding scale for hyperglycemia | |
Docusate sodium / Senna for Constipation | |
Docusate sodium / Senna for Constipation and ondansetron for N/V |
Question 5 Explanation:
LN should be on docusate sodium/Senna for constipation and ondansetron for N/V. Dexamethasone has an off label use for N/V that is chemotherapy-associated. It is mostly used as an anti-inflammatory or immunosuppressant agent. Hydromorphone does not cause hyperglycemia. The most common side effect of opioids are nausea, vomiting and constipation.
Reference:
Dilaudid and Dilaudid HP (hydromorphone) injection package insert. Stamford, CT: Purdue Pharma L.P.; 2016 Oct.
Reference:
Dilaudid and Dilaudid HP (hydromorphone) injection package insert. Stamford, CT: Purdue Pharma L.P.; 2016 Oct.
Question 6 |
LN is 84 YOM who is in hospital for a back surgery.His height is 5 feet and 4 inches, weight 85 kg and NKDA. His past medical history includes hypertension, diabetes mellitus, major depression, hypothyroidism and chronic back pain. Post-op day 1, LN’s medication includes Dexamethasone 8mg iv q6h with taper dosing, Ondansetron 4mg iv q6h prn for N/V, Levothyroxine 0.075mg po daily, Lisinopril 10mg po daily, Citalopram 20mg po daily, Docusate sodium / Senna 1 tab po twice a day, Bisacodyl 10mg suppository daily prn for constipation, Famotidine 20mg iv q12hr, Metoclopramide 10mg iv q6h, Metformin 500mg po bid, D51/2NS with 20K at 125mls/hour and Hydromorphone PCA at 0.2mg/hour of basal rate, demand dose 0.1mg. lock-out every 6min, one hour limit 2.2mg/hour. Pertinent morning labs includes serum creatinine 1.4mg/dl, Mg 1.5mg/dl, K 5.0mmol/L, Na 135mmol/L.
Which of the following medication may increase LN’s potassium?
Ondansetron | |
Metoclopramide | |
Metformin | |
Lisinopril | |
Hydromorphone |
Question 6 Explanation:
Lisinopril may increase LN’s potassium. One of the warnings/precautions of lisinopril is hyperkalemia. ACE inhibitors block the formation of circulating angiotensin II, which can lead to a decrease in aldosterone secretion that can result in an increase in potassium. Risk factors for hyperkalemia while taking lisinopril include renal impairment, diabetes, and concomitant use of potassium-sparing diuretics, potassium supplements and/or potassium containing salts. Potassium should be monitored closely when taking any of the other agents listed. Hyperkalemia is not listed in the warnings/precautions section for the other medications.
Reference:
Raebel MA. Hyperkalemia associated with use of angiotensin-converting enzyme inhibitors and angiotensin receptor blockers.Cardiovasc Ther. 2012 Jun;30(3):e156-66. doi: 10.1111/j.1755-5922.2010.00258.x. Epub 2011 Jan 26.
Reference:
Raebel MA. Hyperkalemia associated with use of angiotensin-converting enzyme inhibitors and angiotensin receptor blockers.Cardiovasc Ther. 2012 Jun;30(3):e156-66. doi: 10.1111/j.1755-5922.2010.00258.x. Epub 2011 Jan 26.
Question 7 |
LN is 84 YOM who is in hospital for a back surgery.His height is 5 feet and 4 inches, weight 85 kg and NKDA. His past medical history includes hypertension, diabetes mellitus, major depression, hypothyroidism and chronic back pain. Post-op day 1, LN’s medication includes Dexamethasone 8mg iv q6h with taper dosing, Ondansetron 4mg iv q6h prn for N/V, Levothyroxine 0.075mg po daily, Lisinopril 10mg po daily, Citalopram 20mg po daily, Docusate sodium / Senna 1 tab po twice a day, Bisacodyl 10mg suppository daily prn for constipation, Famotidine 20mg iv q12hr, Metoclopramide 10mg iv q6h, Metformin 500mg po bid, D51/2NS with 20K at 125mls/hour and Hydromorphone PCA at 0.2mg/hour of basal rate, demand dose 0.1mg. lock-out every 6min, one hour limit 2.2mg/hour. Pertinent morning labs includes serum creatinine 1.4mg/dl, Mg 1.5mg/dl, K 5.0mmol/L, Na 135mmol/L.
What is the reason for holding metformin in patients with reduced renal function?
Metformin can cause acute renal failure | |
Metformin can cause lactic acidosis | |
Metformin can build up neurotoxin | |
Metformin can cause hyperglycemia | |
Metformin can cause hyperkalemia |
Question 7 Explanation:
Metformin is held in patients with reduced renal function due to an increased risk of lactic acidosis. Metformin has a Boxed Warning for lactic acidosis, which is a rare but serious metabolic complication. Lactic acidosis can occurs due to an accumulation of metformin (5 mcg/mL or more). It is fatal in about 50% of cases. Lactic acidosis has also been reported to occur in those with diabetes who have significant renal function impairment. Lactic acidosis occurs when there are elevated blood lactate levels of 5 mmol/L or more, decreased blood pH, electrolyte disturbances with an increased anion gap, and an increased lactate/pyruvate ratio. Normal lactic acid level <2.0 mmol/L
Reference:
Misbin RI. The Phantom of Lactic Acidosis due to Metformin in Patients with Diabetes. Diabetes Care 2004 Jul; 27(7): 1791-1793. https://doi.org/10.2337/diacare.27.7.1791. Accessed Oct 2016
Reference:
Misbin RI. The Phantom of Lactic Acidosis due to Metformin in Patients with Diabetes. Diabetes Care 2004 Jul; 27(7): 1791-1793. https://doi.org/10.2337/diacare.27.7.1791. Accessed Oct 2016
Question 8 |
LN is 84 YOM who is in hospital for a back surgery.His height is 5 feet and 4 inches, weight 85 kg and NKDA. His past medical history includes hypertension, diabetes mellitus, major depression, hypothyroidism and chronic back pain. Post-op day 1, LN’s medication includes Dexamethasone 8mg iv q6h with taper dosing, Ondansetron 4mg iv q6h prn for N/V, Levothyroxine 0.075mg po daily, Lisinopril 10mg po daily, Citalopram 20mg po daily, Docusate sodium / Senna 1 tab po twice a day, Bisacodyl 10mg suppository daily prn for constipation, Famotidine 20mg iv q12hr, Metoclopramide 10mg iv q6h, Metformin 500mg po bid, D51/2NS with 20K at 125mls/hour and Hydromorphone PCA at 0.2mg/hour of basal rate, demand dose 0.1mg. lock-out every 6min, one hour limit 2.2mg/hour. Pertinent morning labs includes serum creatinine 1.4mg/dl, Mg 1.5mg/dl, K 5.0mmol/L, Na 135mmol/L.
It is recommended to monitor complete blood count in patients on chronic metformin because of what reason?
Metformin may decreases erythropoietin level | |
Metformin may decreased platelet count | |
Metformin may decreases vitamin B12 levels | |
Metformin may cause leukocytosis | |
Metformin may decrease iron absorption |
Question 8 Explanation:
Metformin may impair the absorption of vitamin B12, especially in those with inadequate vitamin b12 or calcium intake/absorption. Vitamin b12 deficiency can be treated with discontinuation of therapy or supplementation. Vitamin b12 serum concentrations should be monitored periodically with long-term therapy.
Reference:
Glucophage and Glucophage XR (metformin HCl tablets and extended-release tablets) package insert. Princeton, NJ: Bristol-Myers Squibb Company; 2015 June
Reference:
Glucophage and Glucophage XR (metformin HCl tablets and extended-release tablets) package insert. Princeton, NJ: Bristol-Myers Squibb Company; 2015 June
Question 9 |
LN is 84 YOM who is in hospital for a back surgery.His height is 5 feet and 4 inches, weight 85 kg and NKDA. His past medical history includes hypertension, diabetes mellitus, major depression, hypothyroidism and chronic back pain. Post-op day 1, LN’s medication includes Dexamethasone 8mg iv q6h with taper dosing, Ondansetron 4mg iv q6h prn for N/V, Levothyroxine 0.075mg po daily, Lisinopril 10mg po daily, Citalopram 20mg po daily, Docusate sodium / Senna 1 tab po twice a day, Bisacodyl 10mg suppository daily prn for constipation, Famotidine 20mg iv q12hr, Metoclopramide 10mg iv q6h, Metformin 500mg po bid, D51/2NS with 20K at 125mls/hour and Hydromorphone PCA at 0.2mg/hour of basal rate, demand dose 0.1mg. lock-out every 6min, one hour limit 2.2mg/hour. Pertinent morning labs includes serum creatinine 1.4mg/dl, Mg 1.5mg/dl, K 5.0mmol/L, Na 135mmol/L.
LN used 5 on-demand bolus doses from the hydromorphone PCA, how much hydromorphone did the patient get in 24 hours?
10mg | |
5.3mg | |
4.8mg | |
0.5mg | |
52.8mg |
Question 9 Explanation:
0.2 mg/hour basal rate = 0.2mg/hour (24 hours) = 4.8 mg
Demand dose of 0.1 mg x 5 = 0.5 mg
4.8 mg + 0.5 mg = 5.3 mg
Reference:
Cohen MR. Patient-Controlled Analgesia: Making It Safer for Patients. Institute for Safe Medication Practices (ISMP), May 2006. Retrieved Oct 2016 from: https://www.ismp.org/profdevelopment/PCAMonograph.pdf
Demand dose of 0.1 mg x 5 = 0.5 mg
4.8 mg + 0.5 mg = 5.3 mg
Reference:
Cohen MR. Patient-Controlled Analgesia: Making It Safer for Patients. Institute for Safe Medication Practices (ISMP), May 2006. Retrieved Oct 2016 from: https://www.ismp.org/profdevelopment/PCAMonograph.pdf
Question 10 |
LN is 84 YOM who is in hospital for a back surgery.His height is 5 feet and 4 inches, weight 85 kg and NKDA. His past medical history includes hypertension, diabetes mellitus, major depression, hypothyroidism and chronic back pain. Post-op day 1, LN’s medication includes Dexamethasone 8mg iv q6h with taper dosing, Ondansetron 4mg iv q6h prn for N/V, Levothyroxine 0.075mg po daily, Lisinopril 10mg po daily, Citalopram 20mg po daily, Docusate sodium / Senna 1 tab po twice a day, Bisacodyl 10mg suppository daily prn for constipation, Famotidine 20mg iv q12hr, Metoclopramide 10mg iv q6h, Metformin 500mg po bid, D51/2NS with 20K at 125mls/hour and Hydromorphone PCA at 0.2mg/hour of basal rate, demand dose 0.1mg. lock-out every 6min, one hour limit 2.2mg/hour. Pertinent morning labs includes serum creatinine 1.4mg/dl, Mg 1.5mg/dl, K 5.0mmol/L, Na 135mmol/L.
Which of the following medication’s dose are adjusted for poor renal function?
Famotidine | |
Metoclopramide | |
Lisinopril | |
Citalopram | |
Ondansetron |
Question 10 Explanation:
Famotidine and Metoclopramide would need to be adjusted for poor renal function. Since his CrCl is less than 50, famotidine would need to be adjusted by decreasing the dose by 50% or increasing the interval to every 36 to 48 hours. Metoclopramide would also need to be adjusted by 50% of the normal dose since his CrCl is less than 40. ACEInhibitors and ARBs should be held if serum K is greater than 5.6 or there is a rise in serum creatinine greater than 30% after initiation.
Reference:
Munar, Myrna Y., and Harleen Singh. "Drug dosing adjustments in patients with chronic kidney disease." American family physician 75.10 (2007).
Reference:
Munar, Myrna Y., and Harleen Singh. "Drug dosing adjustments in patients with chronic kidney disease." American family physician 75.10 (2007).
Question 11 |
LN is 84 YOM who is in hospital for a back surgery.His height is 5 feet and 4 inches, weight 85 kg and NKDA. His past medical history includes hypertension, diabetes mellitus, major depression, hypothyroidism and chronic back pain. Post-op day 1, LN’s medication includes Dexamethasone 8mg iv q6h with taper dosing, Ondansetron 4mg iv q6h prn for N/V, Levothyroxine 0.075mg po daily, Lisinopril 10mg po daily, Citalopram 20mg po daily, Docusate sodium / Senna 1 tab po twice a day, Bisacodyl 10mg suppository daily prn for constipation, Famotidine 20mg iv q12hr, Metoclopramide 10mg iv q6h, Metformin 500mg po bid, D51/2NS with 20K at 125mls/hour and Hydromorphone PCA at 0.2mg/hour of basal rate, demand dose 0.1mg. lock-out every 6min, one hour limit 2.2mg/hour. Pertinent morning labs includes serum creatinine 1.4mg/dl, Mg 1.5mg/dl, K 5.0mmol/L, Na 135mmol/L.
The bioavailability of levothyroxine is roughly 50%. The physician requests you for a dose recommendation to convert her home dose of 75mcg po daily to intravenous. What would be the appropriate intravenous dose?
37.5mcg | |
75mcg | |
75mg | |
150mcg | |
37.5mg |
Question 11 Explanation:
Since the bioavailability of levothyroxine is roughly 50% (given in the question).To convert the home dose to intravenous, it would be 50% of the oral dose. So 50% of oral 75 mcg would be 37.5 mcg intravenously.
Reference:
Fish LH, Schwartz HL, Cavanaugh J, et al. Replacement dose, metabolism, and bioavailability of levothyroxine in the treatment of hypothyroidism. N Engl J Med 1987;316:764-70.
Reference:
Fish LH, Schwartz HL, Cavanaugh J, et al. Replacement dose, metabolism, and bioavailability of levothyroxine in the treatment of hypothyroidism. N Engl J Med 1987;316:764-70.
Question 12 |
LN is 84 YOM who is in hospital for a back surgery.His height is 5 feet and 4 inches, weight 85 kg and NKDA. His past medical history includes hypertension, diabetes mellitus, major depression, hypothyroidism and chronic back pain. Post-op day 1, LN’s medication includes Dexamethasone 8mg iv q6h with taper dosing, Ondansetron 4mg iv q6h prn for N/V, Levothyroxine 0.075mg po daily, Lisinopril 10mg po daily, Citalopram 20mg po daily, Docusate sodium / Senna 1 tab po twice a day, Bisacodyl 10mg suppository daily prn for constipation, Famotidine 20mg iv q12hr, Metoclopramide 10mg iv q6h, Metformin 500mg po bid, D51/2NS with 20K at 125mls/hour and Hydromorphone PCA at 0.2mg/hour of basal rate, demand dose 0.1mg. lock-out every 6min, one hour limit 2.2mg/hour. Pertinent morning labs includes serum creatinine 1.4mg/dl, Mg 1.5mg/dl, K 5.0mmol/L, Na 135mmol/L.
Day 3 post-operation LN’s pain was much better and only used 3 mg of hydromorphone in the 24hrs. Physician wants to change to oral morphine. What would be your best recommendation?
Morphine SR 10mg po daily and morphine 5mg po q6h prn for breakthrough pain | |
Morphine 60mg ER po daily and morphine 15mg po q6h prn breakthrough pain | |
Morphine 30mg ER po q6hr and morphine 5mg q6h prn for breakthrough pain | |
Morphine 15mg ER po q12hr and morphine 15mg po q6h prn for breakthrough pain | |
Morphine 15mg ER po q12hr and morphine 5mg po q6h prn breakthrough pain |
Question 12 Explanation:
Since LN used 3 mg of hydromorphone, this would be equivalent to a total of morphine 60 mg po daily. Since you would start with 70-80% of that dose, Morphine 15mg ER po q12hr and morphine 5mg po q6h prn breakthrough pain would be appropriate regimen.
Reference:
American Pain Society. Principles of Analgesic Use in the Treatment of Acute Pain and Cancer Pain, 4th ed. Glenview, Ill. 1999.
Reference:
American Pain Society. Principles of Analgesic Use in the Treatment of Acute Pain and Cancer Pain, 4th ed. Glenview, Ill. 1999.
Question 13 |
LN is 84 YOM who is in hospital for a back surgery.His height is 5 feet and 4 inches, weight 85 kg and NKDA. His past medical history includes hypertension, diabetes mellitus, major depression, hypothyroidism and chronic back pain. Post-op day 1, LN’s medication includes Dexamethasone 8mg iv q6h with taper dosing, Ondansetron 4mg iv q6h prn for N/V, Levothyroxine 0.075mg po daily, Lisinopril 10mg po daily, Citalopram 20mg po daily, Docusate sodium / Senna 1 tab po twice a day, Bisacodyl 10mg suppository daily prn for constipation, Famotidine 20mg iv q12hr, Metoclopramide 10mg iv q6h, Metformin 500mg po bid, D51/2NS with 20K at 125mls/hour and Hydromorphone PCA at 0.2mg/hour of basal rate, demand dose 0.1mg. lock-out every 6min, one hour limit 2.2mg/hour. Pertinent morning labs includes serum creatinine 1.4mg/dl, Mg 1.5mg/dl, K 5.0mmol/L, Na 135mmol/L.
What is LN’s creatinine clearance using Cockcroft and Gault equation based on IBW?
43 mls/min | |
53 mls/min | |
63 mls/min | |
33 mls/min | |
23 mls/min |
Question 13 Explanation:
ABW = 85 kg
IBW = 50 kg + 2.3 kg (4) = 59.2 kg
85/59.2 = 1.44
AdjBW = 59.2 kg + 0.4(85 kg-59.2 kg) = 69.52 kg
CrCl (IBW) = [(140-84) 59.2]/(72 x 1.4) = 32.8
CrCl (AdjBW) = [(140-84) 69.52]/(72 x 1.4) = 38.6
Reference:
Jelliffe RW. Creatinine clearance: Bedside estimate. Ann Inter Med. 1973; 79:604
IBW = 50 kg + 2.3 kg (4) = 59.2 kg
85/59.2 = 1.44
AdjBW = 59.2 kg + 0.4(85 kg-59.2 kg) = 69.52 kg
CrCl (IBW) = [(140-84) 59.2]/(72 x 1.4) = 32.8
CrCl (AdjBW) = [(140-84) 69.52]/(72 x 1.4) = 38.6
Reference:
Jelliffe RW. Creatinine clearance: Bedside estimate. Ann Inter Med. 1973; 79:604
Question 14 |
If LN receives Dextrose 5% half Normal Saline with 20 meq of Potassium as IVF at 125mls/hour. How much dextrose is he getting in 24hrs?
300gm | |
500gm | |
50gm | |
150gm | |
200gm |
Question 14 Explanation:
0.05 (1000 mL) = 50 g
1000 mL x (1 hour/125 mL) = 8 hours
50x 3 = 150 g
1000 mL x (1 hour/125 mL) = 8 hours
50x 3 = 150 g
Question 15 |
You need 51.3 mEq of NaCl to make 1/3 NS 1 liter bag. How many ml of 23.4% NaCl would you need? (Molecular weight of Na is 23 and Cl is 35.5)
12.82ml | |
16.82ml | |
23.4ml | |
58.5ml | |
10ml |
Question 15 Explanation:
1mEq NaCl= 58.5 ; Valence = 1.
mg = mEq x molecular weight / valence.
mg = 51.3mEq x 58.5mg / 1 = 3001.05mg = 3g.
23.4 g/100ml = 3g/Xml
X = 12.825mL
mg = mEq x molecular weight / valence.
mg = 51.3mEq x 58.5mg / 1 = 3001.05mg = 3g.
23.4 g/100ml = 3g/Xml
X = 12.825mL
Question 16 |
Which of the following is/are a risk factor for myopathy with statin therapy?
Hypothyroidism | |
Vitamin D deficiency | |
Renal impairment | |
Hepatic dysfunction | |
Vitamin C deficiency |
Question 16 Explanation:
Risk factors for myopathy are hypothyroidism, reduced renal or hepatic function, rheumatologic disorders such as polymyalgia rheumatica, steroid myopathy, vitamin D deficiency, or primary muscle diseases.
Reference:
Stone N, Robinson J, Lichtenstein A et al. 2013 ACC/AHA Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults. Circulation. 2013;129(25 suppl 2):S1-S45. doi:10.1161/01.cir.0000437738.63853.7a.
Reference:
Stone N, Robinson J, Lichtenstein A et al. 2013 ACC/AHA Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults. Circulation. 2013;129(25 suppl 2):S1-S45. doi:10.1161/01.cir.0000437738.63853.7a.
Question 17 |
Which of the following is considered first-line therapy for reducing the risk of atherosclerotic cardiovascular disease (ASCVD)?
HMG Co-A reductase inhibitors | |
Bile acid resins | |
Nicotinic Acid | |
Fibrates | |
Fish oil |
Question 17 Explanation:
ATP4 found that the use of statins for prevention of ASCVD is extensive and consistent. Statin therapy is recommended for patients at a higher risk of ASCVD who are most likely to experience a net benefit in terms of the potential for risk reduction vs the potential for adverse effects. Non-statin therapies do not provide sufficient benefits in the reduction of ASCVD risk in regards to their potential for adverse effects.
Reference:
Stone N, Robinson J, Lichtenstein A et al. 2013 ACC/AHA Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults. Circulation. 2013;129(25 suppl 2):S1-S45. doi:10.1161/01.cir.0000437738.63853.7a.
Reference:
Stone N, Robinson J, Lichtenstein A et al. 2013 ACC/AHA Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults. Circulation. 2013;129(25 suppl 2):S1-S45. doi:10.1161/01.cir.0000437738.63853.7a.
Question 18 |
If you mix 30 gm 5% lidocaine cream and 90gm of 0.5% hydrocortisone cream, what percent of lidocaine and hydrocortisone do you have as the end product?
Lidocaine/Hydrocortisone 2%/1.25% | |
Lidocaine/Hydrocortisone 0.375%/0.15% | |
Lidocaine/Hydrocortisone 1.25 %/ 0.15% | |
Lidocaine/Hydrocortisone 2% /0.25% | |
Lidocaine/Hydrocortisone 1.25% /0.375% |
Question 18 Explanation:
Lidocaine: 30g x 0.05 = 1.5g.
Hydrocortisone: 90g x 0.005 = 0.45g.
90g+30g = 120g.
1.5g/120g = 0.0125 x100 = 1.25% Lidocaine.
0.45g/120g = 0.00375 x 100 = 0.375% Hydrocortisone.
Hydrocortisone: 90g x 0.005 = 0.45g.
90g+30g = 120g.
1.5g/120g = 0.0125 x100 = 1.25% Lidocaine.
0.45g/120g = 0.00375 x 100 = 0.375% Hydrocortisone.
Question 19 |
In a study where Rivaroxaban was compared to enoxaparin to find total VTE following HIP replacement surgery, there were 17 total VTE out of 1513 patients in the Rivaraoaban group and 57 total VTE out of 1473 patient in the enoxaparin group. What is the relative risk reduction of using Rivaroxaban over Enoxaparin?
39% | |
71% | |
29% | |
14% | |
42% |
Question 19 Explanation:
Relative risk reduction: 0.71 = 71%
Relative risk: (Event rate in rivaroxaban group)/(Event rate in enoxaparin group) = (17/1513)/(57/1473) = 0.2903
Relative risk reduction: 1 – (relative risk) = 1 – 0.2903 = 0.7097 = 0.71
Reference:
I. Barratt A, Wyer PC, Hatala R, et al. Tips for learners of evidence-based medicine: 1. Relative risk reduction, absolute risk reduction and number needed to treat. CMAJ. 2004;171(4):353-8. doi: 10.1503/cmaj.1021197.
II. Stone N, Robinson J, Lichtenstein A et al. 2013 ACC/AHA Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults. Circulation. 2013;129(25 suppl 2):S1-S45. doi:10.1161/01.cir.0000437738.63853.7a.
Relative risk: (Event rate in rivaroxaban group)/(Event rate in enoxaparin group) = (17/1513)/(57/1473) = 0.2903
Relative risk reduction: 1 – (relative risk) = 1 – 0.2903 = 0.7097 = 0.71
Reference:
I. Barratt A, Wyer PC, Hatala R, et al. Tips for learners of evidence-based medicine: 1. Relative risk reduction, absolute risk reduction and number needed to treat. CMAJ. 2004;171(4):353-8. doi: 10.1503/cmaj.1021197.
II. Stone N, Robinson J, Lichtenstein A et al. 2013 ACC/AHA Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults. Circulation. 2013;129(25 suppl 2):S1-S45. doi:10.1161/01.cir.0000437738.63853.7a.
Question 20 |
An order is received for heparin 18 units per kg per hour on a patient whose weight is 125lb. The IV bag comes as a concentration of 50 units /mL. Calculate the infusion rate in terms of mL/hr.
5.15 mls/hr | |
10.23 mls/hr | |
40.9 mls/hr | |
20.45 mls/hr | |
18 mls/hr |
Question 20 Explanation:
125 lb =56Kg, 56Kg x [18 units/ 1 kg] = 1022.72 units/hr,
1022.72 units x [1 mL/50 units] = 20.45 mL/hr
1022.72 units x [1 mL/50 units] = 20.45 mL/hr
Question 21 |
According to the 2013 ACC/AHA Guideline on the Treatment of Blood Cholesterol to ReduceAtherosclerotic Cardiovascular Risk in Adults, which of the following LDL cholesterol thresholds is an indication for high-intensity statin therapy?
≥ 100 mg/dL | |
≥ 130 mg/dL | |
≥ 190 mg/dL | |
≥ 200 mg/dL | |
≥ 150 mg/dL |
Question 21 Explanation:
Statin therapy should be used as treatment in adults with with primary LDL–C ≥190 mg/dL and age over 21 years. Unless contraindicated, high-intensity statin therapy should be used.
Reference:
Stone N, Robinson J, Lichtenstein A et al. 2013 ACC/AHA Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults. Circulation. 2013;129(25 suppl 2):S1-S45. doi:10.1161/01.cir.0000437738.63853.7a.
Reference:
Stone N, Robinson J, Lichtenstein A et al. 2013 ACC/AHA Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults. Circulation. 2013;129(25 suppl 2):S1-S45. doi:10.1161/01.cir.0000437738.63853.7a.
Question 22 |
Injectable Sulfamethoxazole/Trimethoprim comes as 400mg/80mg/5ml. Physician requests you to dose a Sulfamethoxazole/Trimethoprim intravenously for PCP. You know the dose is 15mg/kg/day (based on TMP component) divided q6h. How many milliliters of Sulfamethoxazole/Trimethoprim of 400mg/80mg/5ml would you need for single dose? Patient weighs 80Kg.
18.75 mL | |
75 mL | |
15 mL | |
50 mL | |
16.5 mL |
Question 22 Explanation:
80kg person = 15mg/kg/day = 1200mg/day
80mg /5ml = 1200mg/X
X= 75mL/day / 4 doses = 18.75 mL per dose
80mg /5ml = 1200mg/X
X= 75mL/day / 4 doses = 18.75 mL per dose
Question 23 |
Which of the following is/are appropriate for pseudomonas skin/soft tissue infections?
Ertapenem | |
Cefepime | |
Ceftaroline | |
Cefazolin | |
Vancomycin |
Question 23 Explanation:
Ceftaroline covers MRSA, but it does not cover pseudomonas. Ertapenem does not cover pseudomonas. Cefazolin does not cover MRSA nor Pseudomonas. Cefepime has pseudomonas coverage. Vancomycin does not cover gram negative bacteria.
Reference:
Gilbert D. The Sanford Guide to Antimicrobial Therapy 2014. Sperryville, Va.: Antimicrobial Therapy; 2014
Reference:
Gilbert D. The Sanford Guide to Antimicrobial Therapy 2014. Sperryville, Va.: Antimicrobial Therapy; 2014
Question 24 |
What is the weight of 1000 ml of serum protein whose specific gravity is 1.27?
1270 gm | |
127mg | |
12.7mg | |
12.7gm | |
1.27gm |
Question 24 Explanation:
SG= weight/mL, 1.27 = X/1000ml
X = 1270gm
X = 1270gm
Question 25 |
RL is a 54 YOM who’s calculated 10-year atherosclerotic cardiovascular disease (ASCVD) risk is 18 %. Which of the following is the most appropriate pharmacotherapy recommendation for CR?
Rosuvastatin 10 mg PO QHS | |
Atorvastatin 80 mg PO QHS | |
Lovastatin 10 mg PO QHS | |
Pravastatin 20 mg PO QHS | |
Atorvastatin 20mg PO QHS |
Question 25 Explanation:
This patient belongs in one of the four statin benefit groups because his estimated 10-year ASCVD risk is over 7.5%. Adults 40 to 75 years of age with LDL–C 70 to 189 mg/dL, with an estimated 10-year ASCVD risk ≥7.5% and without clinical ASCVD or diabetes should receive either a moderate-intensity or high-intensity statin. Since the extent of reducing the risk of ASCVD is proportionally related to the degree of LDL-C reduction, risk could be reduced more so with a high intensity statin.Considering the given options, Atorvastatin 80 mg PO QHS is the best choice.
Reference:
Stone N, Robinson J, Lichtenstein A et al. 2013 ACC/AHA Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults. Circulation. 2013;129(25 suppl 2):S1-S45. doi:10.1161/01.cir.0000437738.63853.7a.
Reference:
Stone N, Robinson J, Lichtenstein A et al. 2013 ACC/AHA Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults. Circulation. 2013;129(25 suppl 2):S1-S45. doi:10.1161/01.cir.0000437738.63853.7a.
Question 26 |
What is the mEq/ml (Milliequivalents) of 50% Magnesium Sulfate? (Molecular Weight of MgSO4 is 120.4g/mol).
8.3mEq/ml | |
4.11mEq/ml | |
62mEq/ml | |
50mEq/ml | |
2.06mEq/ml |
Question 26 Explanation:
50% = 50g/100ml = 0.5g/ml = 500mg/ml
mEq = (mg/MW) x valence
= (500mg/120.4) x 2
= 8.3mEq/ml
Question 27 |
All of the following may increase triglycerides except?
Protease inhibitor | |
Bile acid sequestrants | |
Fish Oil | |
Oral estrogens | |
Glucocorticoids |
Question 27 Explanation:
Agents that can cause elevated triglycerides: oral estrogens, glucocorticoids, bile acid sequestrants, protease inhibitors, retinoic acid, anabolic steroids, sirolimus, raloxifene, tamoxifen, beta blockers (not carvedilol), and thiazides.
Reference:
Stone N, Robinson J, Lichtenstein A et al. 2013 ACC/AHA Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults. Circulation. 2013;129(25 suppl 2):S1-S45. doi:10.1161/01.cir.0000437738.63853.7a.
Reference:
Stone N, Robinson J, Lichtenstein A et al. 2013 ACC/AHA Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults. Circulation. 2013;129(25 suppl 2):S1-S45. doi:10.1161/01.cir.0000437738.63853.7a.
Question 28 |
Which of the following is/are ordinal data?
NYHA I-IV | |
Grade of breast cancer | |
Sex | |
Improvement Yes/No | |
Alive or Dead |
Question 28 Explanation:
Categorical data includes ordinal (ordered categories) and nominal (unordered categories). NYHA I-IV and grade of breast cancer are considered ordinal data because the categories for the answer choice are in order, you can have NYHA class I, II, III, or IV. Grade of breast cancers are also in order, grade 1, 2, or 3. Sex, Improvemnet Yes/No, Alive or Dead is considered nominal, unordered data because the answer choices are female or male, and do not have a set order.
Reference:
"Statistics at Square One | The BMJ". Bmj.com. 2016. Web. 7 Nov. 2016. Available at: http://www.bmj.com/about-bmj/resources-readers/publications/statistics-square-one
Reference:
"Statistics at Square One | The BMJ". Bmj.com. 2016. Web. 7 Nov. 2016. Available at: http://www.bmj.com/about-bmj/resources-readers/publications/statistics-square-one
Question 29 |
What is the Osmolarity in mOsm/L of 40mEq of KCl in 100ml sterile water? (Molecular Weight of KCl is 74.5gm/mol)?
400mOsm/L | |
800mOsm/L | |
80mOsm/L | |
200mOsm/L | |
1600mOsm/L |
Question 29 Explanation:
40mEq X 1 equiv/1000mEq X 74.5g/1 equiv = 2.98 gm of KCl in 100ml.
Calculate: mOsm/L.
2.98g/100ml X 1 mol/74.5g x 2Osm/1 mol X 1000mOsm/1 Osm X 1000ml/1L = 800mOsm/L
Calculate: mOsm/L.
2.98g/100ml X 1 mol/74.5g x 2Osm/1 mol X 1000mOsm/1 Osm X 1000ml/1L = 800mOsm/L
Question 30 |
Which of the following medication may increase LDL?
Lisinopril | |
Hydrochlorothiazide | |
Diltiazem | |
Metoprolol | |
Amlodipine |
Question 30 Explanation:
LDL can be elevated by diuretics, cyclosporine, glucocorticoids, and amiodarone.
Reference: Stone N, Robinson J, Lichtenstein A et al. 2013 ACC/AHA Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults. Circulation. 2013; 129(25 suppl 2):S1-S45. doi:10.1161/01.cir.0000437738.63853.7a.
Reference: Stone N, Robinson J, Lichtenstein A et al. 2013 ACC/AHA Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults. Circulation. 2013; 129(25 suppl 2):S1-S45. doi:10.1161/01.cir.0000437738.63853.7a.
Question 31 |
In Normal distribution, what percentage of the sample is found within 2 standard deviation of the mean?
68% | |
95% | |
99% | |
100% | |
72% |
Question 31 Explanation:
In a normal distribution sample, within 1 standard deviation 68% of the sample falls within 1 standard deviation, 95% within 2 standard deviations, and 99.7% within 3 standard deviations of the mean.
Reference:
I. "Mean, Mode And Median - Measures Of Central Tendency - When To Use With Different Types Of Variable And Skewed Distributions | Laerd Statistics". statistics.laerd.com. 2016. Web. 7 Nov. 2016. Available at: https://statistics.laerd.com/statistical-guides/measures-central-tendency-mean-mode-median.php
II. "Statistics at Square One | The BMJ". Bmj.com. 2016. Web. 7 Nov. 2016. Available at: http://www.bmj.com/about-bmj/resources-readers/publications/statistics-square-one
Reference:
I. "Mean, Mode And Median - Measures Of Central Tendency - When To Use With Different Types Of Variable And Skewed Distributions | Laerd Statistics". statistics.laerd.com. 2016. Web. 7 Nov. 2016. Available at: https://statistics.laerd.com/statistical-guides/measures-central-tendency-mean-mode-median.php
II. "Statistics at Square One | The BMJ". Bmj.com. 2016. Web. 7 Nov. 2016. Available at: http://www.bmj.com/about-bmj/resources-readers/publications/statistics-square-one
Question 32 |
A Physician orders amiodarone 1 mg/min for six hours, then 0.5 mg/min thereafter. The patient’s weight is 156 lbs. The concentration of the IV bag comes as 1.8 mg per ml. Calculate the infusion rate in mL/hr.
33.33mls/hr then /16.67mls/hr | |
60mls/hr then 30mls/hr | |
30mls/hr then 15mls/hr | |
16.67mls/hr then 8.3mls/hr | |
8.3mls/hr then 4.15mls/hr |
Question 32 Explanation:
[1 mg/ 1 min] x60min= 60mg/hr. 60 mg/hr x [1 mL/ 1.8 mg] = 33.33 mL/hr
0.5 mg/min x [60 min/ 1 hr] = 30 mg/hr
30 mg/hr x [1 mL/1.8 mg] = 16.67 mL/hr
Infusion rates: 33.33 mL/hr for 6 hours, then 16.67 mL/hr
0.5 mg/min x [60 min/ 1 hr] = 30 mg/hr
30 mg/hr x [1 mL/1.8 mg] = 16.67 mL/hr
Infusion rates: 33.33 mL/hr for 6 hours, then 16.67 mL/hr
Question 33 |
Which of the following medication can lower seizures threshold?
Bupropion | |
Tramadol | |
Clozapine | |
Thiothixene | |
All of the above can lower seizure threshold |
Question 33 Explanation:
Seizure threshold can be lowered by bupropion, chlorpromazine, clozapine, maprotiline, olanzapine, thioridazine, thiothixene, and tramadol.
Reference:
American Geriatrics Society 2015 Updated Beers Criteria for Potentially Inappropriate Medication Use in Older Adults. Journal of the American Geriatrics Society. 2015;63(11):2227-2246. doi:10.1111/jgs.13702.
Reference:
American Geriatrics Society 2015 Updated Beers Criteria for Potentially Inappropriate Medication Use in Older Adults. Journal of the American Geriatrics Society. 2015;63(11):2227-2246. doi:10.1111/jgs.13702.
Question 34 |
Which of the following medication should be avoided in patients with heart failure?
Cilostazol | |
Pioglitazone | |
Naproxen | |
Celebrex | |
All of the above |
Question 34 Explanation:
Patients with heart failure should avoid taking NSAIDs (which includes naproxen), COX-2 inhibitors, nondihydropyridine calcium channel blockers (for reduced EF), thiazolidinediones (which includes pioglitazone), cilostazol, and dronedarone (for severe or recently decompensated heart failure).
Reference:
American Geriatrics Society 2015 Updated Beers Criteria for Potentially Inappropriate Medication Use in Older Adults. Journal of the American Geriatrics Society. 2015;63(11):2227-2246. doi:10.1111/jgs.13702
Reference:
American Geriatrics Society 2015 Updated Beers Criteria for Potentially Inappropriate Medication Use in Older Adults. Journal of the American Geriatrics Society. 2015;63(11):2227-2246. doi:10.1111/jgs.13702
Question 35 |
Which of the following should be monitored when a patient is on SGLT2 inhibitor?
Hydration status | |
Blood pressure | |
Blood glucose | |
Renal function | |
All of the above |
Question 35 Explanation:
Because SGLT2 inhibitors work by preventing reabsorption of glucose in the kidneys, this increases frequency of urination. All of the options are monitoring requirements since the hydration status, blood pressure, blood glucose, and renal function may all be changed from increased urination (from the mechanism of the drug).
Reference:
Garber AJ, et al. Consensus Statement by the American Association of Clinical Endocrinologists and American College of Endocrinology on the Comprehensive Type 2 Diabetes Management Algorithm – 2016 Executive Summary. Endocr Pract. 2016; 22(1):84-113
Reference:
Garber AJ, et al. Consensus Statement by the American Association of Clinical Endocrinologists and American College of Endocrinology on the Comprehensive Type 2 Diabetes Management Algorithm – 2016 Executive Summary. Endocr Pract. 2016; 22(1):84-113
Question 36 |
Which of the following is dichotomous variable?
Sex | |
Pain yes/ Pain no | |
alive / dead | |
Grade of Breast Cancer | |
NYHA I-IV |
Question 36 Explanation:
Dichotomous data is considered categorical data that only has two categories, or two answer choices. All 3 answer choices have only 2 categories: sex has male or female, pain is yes or no, and alive or dead is only two options also.
Reference:
"Statistics at Square One | The BMJ". Bmj.com. 2016. Web. 7 Nov. 2016. Available at: http://www.bmj.com/about-bmj/resources-readers/publications/statistics-square-one
Reference:
"Statistics at Square One | The BMJ". Bmj.com. 2016. Web. 7 Nov. 2016. Available at: http://www.bmj.com/about-bmj/resources-readers/publications/statistics-square-one
Question 37 |
Which of the following antidiabetic medication works by decreasing glucose reabsorption?
Miglitol | |
Linagliptin | |
Pioglitazone | |
Exenatide | |
Empagliflozin |
Question 37 Explanation:
Empagliflozin is a SGLT2 inhibitor to decrease glucose reabsorption in the kidney. Linagliptin is a DPP-4 inhibitor that works on incretins/increase insulin secretion/decrease glucagon secretion. Pioglitazone is a TZD that increases insulin sensitivity. Exenatide is a GLP-1 agonist which increase insulin secretion/decrease glucagon secretion/increase satiety.
Reference: 1. American Diabetes Association. In Standards of Medical Care in Diabetes 2016. Diabetes Care 2016;39(Suppl. 1)
Reference: 1. American Diabetes Association. In Standards of Medical Care in Diabetes 2016. Diabetes Care 2016;39(Suppl. 1)
Question 38 |
If a patient is getting NS IVF at 120mls/hr. How much Sodium Chloride in grams is this patient getting in 24 hours? NS is 0.9% sodium chloride.
25.92gm | |
25.92kg | |
25.92mg | |
90mg | |
90gm |
Question 38 Explanation:
0.9%= 0.9g/100mL, 120mL/h x 24hrs = 2880mL
0.9g/100ml= X/2880ml
X=25.92g of NaCl
0.9g/100ml= X/2880ml
X=25.92g of NaCl
Question 39 |
Which of the following class of antidiabetic medication may cause fluid retention?
Bile acid sequestrant | |
GLP-1 agonist | |
Thiazolidinediones | |
SGLT2 Inhibitor | |
Alpha-glucosidase inhibitor |
Question 39 Explanation:
Thiazolidinediones may cause fluid retention through proposed mechanism of increasing reabsorption in the collecting duct of the kidney and increasing vascular permeability in adipose tissue. Bile acid sequestrants work in the intestine to bind bile acids which doesn’t affect fluid retention. GLP-1 receptor agonists work to activate these receptors to secrete insulin from beta pancreatic cells/decrease glucagon secretion/ increase satiety and doesn’t affect fluid retention. SGLT2 inhibitors actually cause increase of fluid elimination through the kidneys. Alpha-glucosidase inhibitors work in the gut to decrease carb absorption/digestion and have no affect on fluid retention.
Reference:
I. Yang T, Soodvilai S. Renal and Vascular Mechanisms of Thiazolidinediones- Induced Fluid Retention. PPAR Research. 2008. Article ID 943614.
II. American Diabetes Association. In Standards of Medical Care in Diabetes 2016. Diabetes Care 2016;39(Suppl. 1)
Reference:
I. Yang T, Soodvilai S. Renal and Vascular Mechanisms of Thiazolidinediones- Induced Fluid Retention. PPAR Research. 2008. Article ID 943614.
II. American Diabetes Association. In Standards of Medical Care in Diabetes 2016. Diabetes Care 2016;39(Suppl. 1)
Question 40 |
Which of the following medication should be avoided if a patient is on lithium to avoid lithium toxicity?
Lisinopril | |
Furosemide | |
Naproxen | |
Amiodarone | |
Warfarin |
Question 40 Explanation:
ACE-inhibitors (such as lisinopril), NSAIDs (such as naproxen) and loop diuretics (furosemide) can all increase the risk of lithium toxicity.
Reference:
American Geriatrics Society 2015 Updated Beers Criteria for Potentially Inappropriate Medication Use in Older Adults. Journal of the American Geriatrics Society. 2015;63(11):2227-2246. doi:10.1111/jgs.13702.
Reference:
American Geriatrics Society 2015 Updated Beers Criteria for Potentially Inappropriate Medication Use in Older Adults. Journal of the American Geriatrics Society. 2015;63(11):2227-2246. doi:10.1111/jgs.13702.
Question 41 |
Which of the following class of antidiabetic medications can increase triglycerides?
Bile acid sequestrant | |
GLP-1 agonist | |
Thiazolidinediones | |
SGLT2 Inhibitor | |
Alpha-glucosidase inhibitors |
Question 41 Explanation:
The only bile acid sequestrant, colesevelam (Welchol), has been shown to increase triglycerides through mechanism of: activation of phosphatidic acid phosphatase with promotes triglyceride synthesis. GLP-1 agonists work on GLP 1 receptors to increase insulin secretion, decrease glucagon secretion, and increase satiety. Thiazolidinediones activate nuclear transcription factor PPAR gamma to increase insulin sensitivity. SGLT2 inhibitors inhibit glucose reabsorption in the kidney. Alpha-glucosidase inhibitors slow down digestion and absorptions of carbs in the gut.
Reference: 1. Welchol (colesevelam) tablets and powder for oral suspension package insert. Parsipanny, NJ: Daiiki Sankyo 2014.
2. Sheperd J. Mechanism of action of bile acid sequestrants and other lipid-lowering drugs. Cardiology. 1989; 76 Suppl 1:65-71; discussion 71-74.
Reference: 1. Welchol (colesevelam) tablets and powder for oral suspension package insert. Parsipanny, NJ: Daiiki Sankyo 2014.
2. Sheperd J. Mechanism of action of bile acid sequestrants and other lipid-lowering drugs. Cardiology. 1989; 76 Suppl 1:65-71; discussion 71-74.
Question 42 |
A Physician orders Dobutamine HCl IV infusion at 5 mcg/kg/min. Dobutamine HCl is available as 500 mg in 250 mL of D5W. The patient weighs 68 kg. Calculate the infusion rate in mL/hr.
10.2mls/hr | |
5.2mls/hr | |
0.17mls/hr | |
22.4mls/hr | |
340mls/hr |
Question 42 Explanation:
68 kg x [5 mcg/kg/min] = 340 mcg/min
Bag concentration = 2 mg/ml or 2000 mcg/ml
340 mcg x [1 mL/2000 mcg] = 0.17 mL/min
60 in x [0.17 mL/min] = 10.2 mLs in one hour
Bag concentration = 2 mg/ml or 2000 mcg/ml
340 mcg x [1 mL/2000 mcg] = 0.17 mL/min
60 in x [0.17 mL/min] = 10.2 mLs in one hour
Question 43 |
When does the newer chronic kidney disease (CKD) guidelines recommend stopping metformin?
when the estimated glomerular filtration (eGFR) is <30 mL/min/1.73 m2 | |
when estimated glomerular filtration (eGFR) is <50 mL/min/1.73 m2 | |
when creatinine clearance <30 ml/min | |
when creatinine clearance <50 ml/min | |
when serum creatinine is <1.8 mg/dL |
Question 43 Explanation:
Metformin should be stopped when eGFR falls below 30. This is the only cutoff that is recommended for absolute discontinuing. If the eGFR falls between 30-44 while ontherapy, benefits and risks of discontinuing should be evaluated. New initiation is only recommended when eGFR >45.
Reference:
I. US Food and Drug Administration (FDA) MedWatch for Metformin-containing Drugs: Revised Warnings for Certain Patients With Reduced Kidney Function. Retrieved April 8, 2016. Available at: http://www.fda.gov/Safety/MedWatch/SafetyInformation/SafetyAlertsforHumanMedicalProducts/ucm494829.htm?source=govdelivery&utm_medium=email&utm_source=govdelivery
II. Eknoyan G, Lameire N, et al. KDIGO 2012 Clinical Practice Guideline for the Evaluation and Management of Chronic Kidney Disease. Journal of International Society of Nephrology. Jan 2013;3(1): 91-111
Reference:
I. US Food and Drug Administration (FDA) MedWatch for Metformin-containing Drugs: Revised Warnings for Certain Patients With Reduced Kidney Function. Retrieved April 8, 2016. Available at: http://www.fda.gov/Safety/MedWatch/SafetyInformation/SafetyAlertsforHumanMedicalProducts/ucm494829.htm?source=govdelivery&utm_medium=email&utm_source=govdelivery
II. Eknoyan G, Lameire N, et al. KDIGO 2012 Clinical Practice Guideline for the Evaluation and Management of Chronic Kidney Disease. Journal of International Society of Nephrology. Jan 2013;3(1): 91-111
Question 44 |
A Physician orders Dopamine 5 mcg/kg/min. The concentration of the Dopamine IV bag is 400 mg in 250 D5W. The patient’s weight is 168 lbs. Calculate the infusion rate in mL/hr.
10.2mls/hr | |
5.2mls/hr | |
14.29mls/hr | |
22.4mls/hr | |
0.17mls/hr |
Question 44 Explanation:
Pt’s weight in Kg 76.4.
76.4 x [5 mcg/kg/min] = 381.18 mcg/min
Concentration of the bag [400 mg/250 mL] = 1.6 mg/ml or 1600mcg
381.18 mcg x [1 mL/1600 mcg] = 0.2382 mL/ml
60 in x [0.0.2382 mL/min] = 14.29 mL in one hour
76.4 x [5 mcg/kg/min] = 381.18 mcg/min
Concentration of the bag [400 mg/250 mL] = 1.6 mg/ml or 1600mcg
381.18 mcg x [1 mL/1600 mcg] = 0.2382 mL/ml
60 in x [0.0.2382 mL/min] = 14.29 mL in one hour
Question 45 |
Which of the following antidiabetic medication works by inhibiting carbohydrate breakdown?
Acarbose | |
Metformin | |
Dapagliflozin | |
Pioglitazone | |
Sitagliptin |
Question 45 Explanation:
Acarbose is an alpha glucosidase inhibitor that inhibits carbohydrate breakdown. Metformin is a biguanide that decreases hepatic glucose production. Dapagliflozin is a SGLT2 inhibitor to decrease glucose reabsorption in the kidney. Pioglitazone is a TZD that increases insulin sensitivity. Sitagliptin is a DPP-4 inhibitor that works on incretins/increase insulin secretion/decrease glucagon secretion.
Reference:
American Diabetes Association. In Standards of Medical Care in Diabetes 2016. Diabetes Care 2016;39(Suppl. 1)
Reference:
American Diabetes Association. In Standards of Medical Care in Diabetes 2016. Diabetes Care 2016;39(Suppl. 1)
Question 46 |
Which of the following would you use for aspiration pneumonia with an intention to cover anaerobes?
Piperacillin-Tazobactam | |
Cefepime | |
Ampicillin-sulbactam | |
Cefazolin | |
Levofloxacin |
Question 46 Explanation:
Cefepime, levofloxacin, cefazolin does not provide good coverage of anaerobes. Ampicillin-sulbactam and piperacillin-tazobactam provide anaerobic coverage.
Reference:
Gilbert D. The Sanford Guide to Antimicrobial Therapy 2014. Sperryville, Va.: Antimicrobial Therapy; 2014.
Reference:
Gilbert D. The Sanford Guide to Antimicrobial Therapy 2014. Sperryville, Va.: Antimicrobial Therapy; 2014.
Question 47 |
You get an order for 5% amino acid 15% dextrose premixed parenteral nutrition solution, 2 L at 83mls/hr. Your pharmacy technician tells you there is manufacture’s backorder on those. How many ml of 20% dextrose would you need to provide the same amount of dextrose in 24 hrs?
1000ml | |
1400ml | |
1500ml | |
200ml | |
2500ml |
Question 47 Explanation:
15% dextrose = 15gm/100ml = 300gm/2000ml. Patient needs 300gm.
300gm/Xml = 20gm/100ml = 1500ml
300gm/Xml = 20gm/100ml = 1500ml
Question 48 |
A physician orders 300gms of albumin post paracentesis, how many milliliters of 25% albumin do you need to give 300gms?
300ml | |
25ml | |
100ml | |
1200ml | |
1000ml |
Question 48 Explanation:
25g/100ml = 300g/Xml
Xml = 1200mL
Xml = 1200mL
Question 49 |
Which of the following antidiabetic medication may cause cyanocobalamin deficiency?
Saxagliptin | |
Canagliflozin | |
Pioglitazone | |
Glimepiride | |
Metformin |
Question 49 Explanation:
Metformin is associated with vitamin B12 deficiency because it affects the calcium dependent membrane uptake of it. All other drug classes are not associated with this.
Reference:
Liu KW, Lok KD, Jean W. Metformin-related vitamin B12 deficiency. Age Aging. 2006. 35(2): 200-201.
Reference:
Liu KW, Lok KD, Jean W. Metformin-related vitamin B12 deficiency. Age Aging. 2006. 35(2): 200-201.
Question 50 |
Octreotide 50mcg/hr is ordered for a patient with esophageal varices, nurses prepared by mixing 1ml of concentration 0.5mg/ml of octreotide in 50mls NS. What rate should the bag be infused?
50ml/hr | |
5ml/hr | |
5ml/min | |
0.5ml/min | |
7ml/hr |
Question 50 Explanation:
The concentration is the first thing to calculate, using 1 mL of octreotide solution containing a concentration of 0.5mg/mL is really using 0.5mg of octreotide. If this is placed in 50 mL NS then it is 0.5mg/50mL which is 0.01mg/mL or 10 mcg/mL. If the patient needs 50 mcg of octreotide per hour then the patient will need 5, 10 mcg/mL doses or 5 mLs. So the rate for this patient would be 5 mL/hr.
Question 51 |
Which of the following beta-blocker is NOT proven to reduce mortality in patients with Systolic CHF?
Bisoprolol
| |
Nadolol
| |
Carvedilol
| |
Metoprolol succinate
| |
Metoprolol Tartrate |
Question 51 Explanation:
Nadolol is not proven to reduce mortality in patients with systolic CHF. The efficacy of nadolol in HF has not been determined. For patients taking nadolol, it should be used with caution in those with compensated heart failure and patients should be monitored for a worsening of the condition.
Bisoprolol, carvedilol, and sustained-release metoprolol succinate are the beta-blockers that have been proven to reduce mortality in patients with systolic CHF. These 3 beta-blockers have been effective in reducing the risk of death in patients with chronic HFrEF. Other beta-blockers were found to be less effective. Bucindolol did not exhibit uniform effectiveness across different populations. Metoprolol tartrate was found to be less effective in HF clinical trials.
Reference:
Yancy CW, Jessup M, Bozkurt B, et al. 2013 ACCF/AHA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines.J Am Coll Cardiol. 2013;62(16):e147-e239. doi:10.1016/j.jacc.2013.05.019. Retirved on Feb 6th from :http://circ.ahajournals.org/content/128/16/e240
Reference:
Yancy CW, Jessup M, Bozkurt B, et al. 2013 ACCF/AHA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines.J Am Coll Cardiol. 2013;62(16):e147-e239. doi:10.1016/j.jacc.2013.05.019. Retirved on Feb 6th from :http://circ.ahajournals.org/content/128/16/e240
Question 52 |
Alteplase is ordered for a 72 YOM who weighs 68kg for Ischemic stroke. The ER physician would like you to dose. As an ER pharmacist you know the dose is 0.9 mg/kg IV (not to exceed 90 mg); give 10% of the total dose as an IV bolus over 1 minute, then give the remaining 90% as an IV infusion over 60 minutes. After reconstitution, the concentration of Altaplace is 1mg/ml. How many ml is needed for the bolus and how many ml is needed for the infusion? Round to the nearest ml.
6ml IV bolus, followed by 55mL IV over 60 minutes
| |
4ml IV bolus, followed by 57mL IV over 60 minutes
| |
3ml IV bolus, followed by 58mL IV over 60 minutes
| |
8ml IV bolus, followed by 52mL IV over 60 minutes
| |
9ml IV bolus, followed by 82mL IV over 60 minutes |
Question 52 Explanation:
68kg x 0.9mg/kg = 61.2mg dose x 1mg/mL = 61.2mL
61.2mg x 0.1 = 6mL IV bolus 61.2mg x 0.9 = 55mL IV over 60 minutes
Question 53 |
TM is a 78 YOW with a history of hypertension, hypercholesterolemia and arthritis was admitted for proximal arterial fibrillation. While in the hospital she was placed on diltiazem drip and eventually, converted to oral diltiazem 240mg. Pt’s home medication includes Simvastatin 40mg po daily , hydrochlorothiazide 25mg po daily , Lisinopril 20mg daily and Acetaminophen. Her LDL-C is 100mg /dL. What would be the most appropriate change to make on her therapy?
Increase Simvastatin to 80mg po daily
| |
Keep Simvastatin at 40mg po daily
| |
Change Simvastatin 40mg to Atorvastatin 40mg po daily
| |
Change Simvastatin to Lovastatin 20mg po daily
| |
Discontinue Statins. |
Question 53 Explanation:
Diltiazem has a major drug interaction with Simvastatin. Diltiazem is a CYP3A4 inhibitor, and since Simvastatin is metabolized by CYP3A4, its level can build up and the risk of myopathy increases. It is recommended to switch to a non-CYP3A inhibitor such as Pitavastatin, Pravastatin, or Rosuvastatin, and if Simvastatin is to be kept on it should not exceed 10 mg/day. The same interaction also exists with lovastatin, and the recommendation is to not exceed a total dose of 20 mg/day po of Lovastatin. Given the current options, the best choice is to change to Atorvstatin 40 mg po daily.
Reference:
I. FDA Drug Safety Communication: New restrictions, contraindications, and dose limitations for Zocor (simvastatin) to reduce the risk of muscle injury. December 15, 2011. Retrieved on Feb 8th, 2017 from : http://www.fda.gov/Drugs/DrugSafety/ucm256581.htm
II. Stone N, Robinson J, Lichtenstein A et al. 2013 ACC/AHA Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults. Circulation. 2013;129(25 suppl 2):S1-S45. doi:10.1161/01.cir.0000437738.63853.7a. Retrieved on Feb 6th 2017 from : http://circ.ahajournals.org/content/129/25_suppl_2/S1
Reference:
I. FDA Drug Safety Communication: New restrictions, contraindications, and dose limitations for Zocor (simvastatin) to reduce the risk of muscle injury. December 15, 2011. Retrieved on Feb 8th, 2017 from : http://www.fda.gov/Drugs/DrugSafety/ucm256581.htm
II. Stone N, Robinson J, Lichtenstein A et al. 2013 ACC/AHA Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults. Circulation. 2013;129(25 suppl 2):S1-S45. doi:10.1161/01.cir.0000437738.63853.7a. Retrieved on Feb 6th 2017 from : http://circ.ahajournals.org/content/129/25_suppl_2/S1
Question 54 |
A patient who weighs 80kg is ordered Esmolol at 50mcg/kg/min. Esmolol comes in 2500mg/250 ml NS premixed bags. What is the infusion rate in mls/hr?
20mls/hr
| |
6mls/hr
| |
8mls/hr
| |
24mls/hr
| |
32mls/hr |
Question 54 Explanation:
50 mcg/kg/min x 80 kg = 4 mg/min x 60 min/hr = 240 mg/hr 2500 mg / 250 mL = 10 mg/mL
240 mg/hr / 10 mg/mL = 24 mL/hr Esmolol Infusion
Question 55 |
WM did not receive influenza vaccine prior to the start of this season, it’s now December. He did get influenza vaccine last year. Which of the following is correct course of action?
Skip influenza vaccine for this year since it’s too late.
| |
Skip influenza vaccine for this year since he received vaccine last year.
| |
Start WM on Tamiflu to prevent him from getting influenza.
| |
Vaccinate him with influenza vaccine since influenza season lasts until March in your community.
| |
Start Amantadine 200mg daily |
Question 55 Explanation:
Influenza vaccine is recommended annually, thus, WM should not skip it this year, and B is incorrect. Also, per the CDC, seasonal influenza outbreaks can occur as early as October, however, most activity peaks in January or later. Thus, it is not too late for WM to receive his vaccine in December, thus A is incorrect. Lastly, antiviral medications such as Tamiflu are an important adjunct to vaccinations. They are recommended as early as possible for any patient with confirmed or suspected influenza who, is 1) Hospitalized, 2) has severe, complicated, or progressive illness or 3) is at higher risk for influenza complications. Thus, WM is not a candidate with the given information and C is incorrect. Starting Tamiflu or Amantadine is not recommended for prevention. It has indication for treatment and prophylaxis.
Reference:
Key Facts About Seasonal Flu Vaccine. Centers for Disease Control and Prevention. 2016. Available at: http://www.cdc.gov/flu/protect/keyfacts.htm. Accessed September 27, 2016.
Reference:
Key Facts About Seasonal Flu Vaccine. Centers for Disease Control and Prevention. 2016. Available at: http://www.cdc.gov/flu/protect/keyfacts.htm. Accessed September 27, 2016.
Question 56 |
FT is a 23 year old newly diagnosed type I diabetes admitted to the hospital due to diabetes ketoacidosis. 2 days after being on insulin drip, anion gap is closed. Physician would like your help in transitioning her to subcutaneous insulin. She suggests using insulin glargine once a day and Insulin lispro three time a day at ratio of 70:30. 70 % of long and 30 % of short acting insulin. FT received average of 70 units of insulin in 24hrs. Which of the following would be the best insulin regimen?
49 units of Insulin Glargine subcutaneous daily and 7 units of Insulin Lispro subcutaneous three times a day with meals
| |
25 units of Insulin Glargine subcutaneous daily and 15 units of Insulin Lispro subcutaneous three times a day with meals
| |
40 units of Insulin Glargine subcutaneous daily and 10 units of Insulin Lispro subcutaneous three times a day with meals
| |
46 units of Insulin Glargine subcutaneous daily and 8 units of Insulin Lispro subcutaneous three times a day with meals
| |
52 units of Insulin Glargine subcutaneous daily and 6 units of Insulin Lispro subcutaneous three times a day with meals |
Question 56 Explanation:
70% of 70 units = 49 units of Insulin Glargine daily
30% of 70 units = 21 units of Insulin Lispro daily. Dived in 3 doses would be 7 units three times a day.
FT’s Insulin regimen should be 49 units of Insulin Glargine subcutaneous daily and 7 units of Insulin Lispro subcutaneous three times a day with meals
Question 57 |
In the US Nurses’ Health Study (NHS) cohort study, where they looked at association of regular aspirin use (≥two 325 mg tablets/week) and colorectal cancer in 82,911 women found (RR, 0.77; 95% CI, 0.67–0.88) over 20 years of follow-up. In an another analysis of the NHS, regular aspirin use, investigator also found (hazard ratio [HR]=0.72, 95% CI 0.56–0.92), what does this say about the mortality from colorectal cancer?
How can this data best be interpreted?
Those who takes aspirin ≥2 times/week have 23% lower risk of colorectal cancer
| |
Those who takes aspirin ≥2 times/week have 0.77% lower risk of colorectal cancer
| |
Those who takes aspirin ≥2 times/week have 28% lower risk of colorectal cancer | |
Those who takes aspirin ≥2 times/week have 23% reduction in death from colorectal cancer
| |
None of the above is correct |
Question 57 Explanation:
Relative risk can be stated as 0.77 times as likely or 0.77 times the risk, but it could also be illustrated as a relative risk reduction and stated as a 23% risk reduction or 23% lower risk by taking the medication.
Reference:
Irwig, Les. Chapter 18: Relative risk, relative and absolute risk reduction, number needed to treat and confidence intervals. Smart health choices: making sense of health advice. Judy Irwig, 2007. Retrieved Jan. 24, 2017 from: https://www.ncbi.nlm.nih.gov/books/NBK63647/
Reference:
Irwig, Les. Chapter 18: Relative risk, relative and absolute risk reduction, number needed to treat and confidence intervals. Smart health choices: making sense of health advice. Judy Irwig, 2007. Retrieved Jan. 24, 2017 from: https://www.ncbi.nlm.nih.gov/books/NBK63647/
Question 58 |
The rate that an outcome will occur given a particular exposure, compared to the rate of the outcome occurring in the absence of that exposure is definition of which of the following?
Incidence rate
| |
Prevelance rate
| |
Odds ratio
| |
Relative risk
| |
Confidence Interval |
Question 58 Explanation:
RR = rate of an outcome occurring in an exposed group (treatment group/intervention group) divided by the rate of an outcome occurring in an unexposed group (control group)
Ex: Relative Risk = Rate of UTI in patients taking drug XYZ / rate of UTI in patients not on drug XYZ
Reference:
I. 2x2 Contingency Table with Odds Ratios, etc. (n.d.). Retrieved Jan. 24, 2017 from: http://www.vassarstats.net/odds2x2.html
II. Szumilas, M. "Explaining odds ratios." J Can Acad Child Adolesc Psychiatry 19 (2010): 227. Retrieved Jan. 24, 2017 from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2938757/
Reference:
I. 2x2 Contingency Table with Odds Ratios, etc. (n.d.). Retrieved Jan. 24, 2017 from: http://www.vassarstats.net/odds2x2.html
II. Szumilas, M. "Explaining odds ratios." J Can Acad Child Adolesc Psychiatry 19 (2010): 227. Retrieved Jan. 24, 2017 from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2938757/
Question 59 |
JM is a 32 year old women who comes to your diabetic clinic with complain of several episodes of hypoglycemia. She is on Insulin NPH/regular 70/30, 22 units twice a day with breakfast and dinner. 8 units with lunch. After discussing with physician you decide to decrease the total daily insulin by 10% and change to insulin glargine once a day and Insulin Lispro three time a day at ratio of 50:50. 50 % of long and 50 % of short acting insulin. What is her new insulin regimen? Round down to the nearest 1 unit.
16 units of insulin glargine once daily, Insulin Lispro 4 units 3 times a day with meals
| |
15 units of insulin glargine once daily, Insulin Lispro 5 units 3 times a day with meals
| |
23 units of insulin glargine once daily, Insulin Lispro 7 units 3 times a day with meals
| |
30 units of insulin glargine once daily, Insulin Lispro 6 units 3 times a day with meals
| |
18 units of insulin glargine once daily, Insulin Lispro 6 units 3 times a day with meals |
Question 59 Explanation:
22 x 2 + 7 = 51 units of total insulin per day
Decrease by 10%
51 units x 0.9 = 45.9 units per day round up to 46 units
46 units x 0.50 = 23 units, administer 23 units of insulin glargine once daily
46 units x 0.50 = 23 units total Insulin Lispro. Round down, divided by three times a day, 7 units 3 times a day with meals
Question 60 |
JK is a 67 years African American man who presents to your clinic for his blood pressure management. His past medical history includes Peptic ulcer disease and hypertension. His two BP readings are 160/98, 159/96 and HR 85. He says he has been adherent to his medication and lifestyle. He currently takes 12.5mg Chlorthalidone and Prilosec 20mg daily. Which of the following is the best strategy to manage his blood pressure?
Increase chlorthalidone to 25mg daily
| |
Add Norvasc 2.5 daily
| |
Add Lisinopril 5mg daily
| |
Add hydrochlorothiazide 25mg daily
| |
Add Lisinopril 20mg daily |
Question 60 Explanation:
As the patient is over the age of 60 and he does not have CKD or diabetes, his goal BP should be SBP < 150 mmHg or DBP < 90 mmHg, and he is not currently at this goal with his medication regimen. Options are to maximize the current medication dosage (option A), or to add a second agent. Since calcium channel blockers like Norvasc are recommended as initial treatment options in African Americans, choosing Norvasc over lisinopril would probably be the more effective option.
Reference:
James P, Oparil S, Carter B et al. 2014 Evidence-Based Guideline for the Management of High Blood Pressure in Adults. JAMA. 2014;311(5):507. doi:10.1001/jama.2013.284427. Retrieved Jan. 24, 2017 from: http://jamanetwork.com/journals/jama/fullarticle/1791497
Reference:
James P, Oparil S, Carter B et al. 2014 Evidence-Based Guideline for the Management of High Blood Pressure in Adults. JAMA. 2014;311(5):507. doi:10.1001/jama.2013.284427. Retrieved Jan. 24, 2017 from: http://jamanetwork.com/journals/jama/fullarticle/1791497
Question 61 |
Results from a Meta-analysis where they looked at frequency of postoperative arterial fibrillation in patients on Ascorbic acid after cardiac surgery found odds ratio, 0.44 (95% CI, 0.32 to 0.61). How can you interpret this data?
Ascorbic acid increased frequency of postoperative arterial fibrillation after cardiac surgery by 44%
| |
Ascorbic acid decreased frequency of postoperative arterial fibrillation after cardiac surgery by 44%
| |
There was no statistically significant difference in frequency of postoperative arterial fibrillation after cardiac surgery
| |
Ascorbic acid decreased frequency of postoperative arterial fibrillation after cardiac surgery by 56%
| |
None of the above are correct |
Question 61 Explanation:
Odds ratio of 0.44 (44%) means that this group was associated with an event happening 44% of the time, compared to 1 (an event happening 100% of the time if unexposed), therefore 100 - 44 = 56%, which is the reduction caused by the exposure. Exposure is the use of ascorbic acid.
Reference:
Davies, Huw Talfryn Oakley, Iain Kinloch Crombie, and Manouche Tavakoli. "When can odds ratios mislead?." Bmj 316.7136 (1998): 989-991. Retrieved Jan. 24, 2017 from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1112884/
Reference:
Davies, Huw Talfryn Oakley, Iain Kinloch Crombie, and Manouche Tavakoli. "When can odds ratios mislead?." Bmj 316.7136 (1998): 989-991. Retrieved Jan. 24, 2017 from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1112884/
Question 62 |
A patient takes 1gm of Calcium Carbonate salt three times a day. How much elemental calcium, in grams, is he getting in 24hrs? (MW of Ca: 40.078 g/mol, MW of CaCO3: 100.087 g/mol)
3 g
| |
1.8g
| |
1.2g
| |
0.8gm
| |
1.8mg |
Question 62 Explanation:
Calcium makes up 40% of the MW of CaCO3.
MW Ca / MW CaCO3
40.078 / 100.087 x 100% = 40%
40% of 1 g CaCO3 = 0.4 g
Patient is taking 0.4 g of Ca 3 times daily
0.4 g Ca x 3 = 1.2 g of Elemental Ca
Question 63 |
Number of new cases per population at risk in a given time period is a definition of which of the following?
Incidence rate
| |
Prevalence rate
| |
Mortality rate
| |
Odds ratio
| |
Confidence Interval |
Question 63 Explanation:
Incidence rate = New reported cases / summed person-years of observation (avg population during time interval). Prevalence = Cases in a population in a given time period / total population at that time Mortality rate = deaths during specified time interval / population size at risk for death
Reference:
Dicker, R. C., Coronado, F., Koo, D., et al. Principals of Epidemiology in Public Health Practice, Third Edition: An Introduction to Applied Epidemiology and Biostatistics; Lesson 3, Section 2. Oct. 2006 Retrieved Jan. 24, 2017 from: https://www.cdc.gov/ophss/csels/dsepd/ss1978/lesson3/section2.html Updated: Nov. 2011
Reference:
Dicker, R. C., Coronado, F., Koo, D., et al. Principals of Epidemiology in Public Health Practice, Third Edition: An Introduction to Applied Epidemiology and Biostatistics; Lesson 3, Section 2. Oct. 2006 Retrieved Jan. 24, 2017 from: https://www.cdc.gov/ophss/csels/dsepd/ss1978/lesson3/section2.html Updated: Nov. 2011
Question 64 |
What is the Osmolarity of NS with KCL 40 meq/L? (MW of KCl: 74.55 g/mol) (MW of NaCl: 58.44 g/mol)
800 mOsm/L
| |
308 mOm/L
| |
1108 mOsm/L
| |
830 mOsm/L
| |
388 mOsm/L |
Question 64 Explanation:
KCl:
Osmoles = number of particles in solution
Convert 40meq to weight in g:
40meq x 1equiv/1000 mEq x 74.5g/1 equiv = 2.98g of KCL
Calculate mOsm/L :
2.98g/L x 1mol/74.5g x 2Osm/1 mol x 1000mOsm/1 Osm = 80mOsm/L
NaCl: 0.9g/100ml x 1mol/58.5 g x 2 Osm/1mol x 1000 mOsm/ 1Osm x 1000ml/1L = 308 mOsm/L 80 mOsm/L + 308 mOsm/L = 388 mOsm/L
NaCl: 0.9g/100ml x 1mol/58.5 g x 2 Osm/1mol x 1000 mOsm/ 1Osm x 1000ml/1L = 308 mOsm/L 80 mOsm/L + 308 mOsm/L = 388 mOsm/L
Question 65 |
CJ is a 69 year old male with a history of diabetes, hypertension and hypercholesterolemia. His fasting lipid profile is TC 530 mg/dL; LDL-C 125; HDL-C 48 mg/dL; and TG 640 mg/dL. His A1c 8.1, calculate creatinine clearance is 65mls/hr, BP 135/80 mm Hg, HR 70 beats /min. His current medications includes metformin 1000mg po bid, lisinopril 20mg daily, sitagliptin 50mg bid and atorvastatin 40mg daily. What is the best pharmacological agent to initiate on CJ?
Increase atorvastatin to 80mg
| |
Niacin 500mg twice daily
| |
Fenofibrate 162mg daily
| |
Gemfibrozil 600mg twice daily
| |
Fish oil 500mg twice daily |
Question 65 Explanation:
It is reasonable to add triglyceride-lowering medications such as fibrates or niacin to prevent pancreatitis in those with triglyceride levels >500 mg/dL, which applies to this patient as his TG level is 640 mg/dL . C. is wrong because gemfibrozil should not be initiated in patients on statin therapy because of an increased risk for muscle symptoms and rhabdomyolysis. Fenofibrate may be considered concomitantly with a low- or moderate- intensity statin when triglycerides are above 500 mg/dL,2, however he is on a high intensity statin therapy. For niacin, the IR dose should start at 100 mg TID2 and niacin does not lower triglyceride levels as much as fibrate do.4 Fenofibrates are dose adjusted for renal function lower than 60 mL/min to 54 mg/mL, so this dose is appropriate for this patient because of his renal function being above 60 mL/min. The best option is fenofibrate 162 mg daily, but this needs to be monitored for any symptoms of muscle pain exhibited by the patient, especially as the patient is at a higher risk due to being a diabetic. Fish oil is not a first line agent to treat hypertriglyceridemia.
Reference: Stone N, Robinson J, Lichtenstein A et al. 2013 ACC/AHA Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults. Circulation. 2013;129(25 suppl 2):S1-S45. doi:10.1161/01.cir.0000437738.63853.7a. Retrieved on Feb 6th 2017 from : http://circ.ahajournals.org/content/129/25_suppl_2/S1
Miller M, Stone N, Ballantyne C et al. Triglycerides and Cardiovascular Disease: A Scientific Statement From the American Heart Association. Circulation. 2011;123(20):2292-2333. doi:10.1161/cir.0b013e3182160726.
Reference: Stone N, Robinson J, Lichtenstein A et al. 2013 ACC/AHA Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults. Circulation. 2013;129(25 suppl 2):S1-S45. doi:10.1161/01.cir.0000437738.63853.7a. Retrieved on Feb 6th 2017 from : http://circ.ahajournals.org/content/129/25_suppl_2/S1
Miller M, Stone N, Ballantyne C et al. Triglycerides and Cardiovascular Disease: A Scientific Statement From the American Heart Association. Circulation. 2011;123(20):2292-2333. doi:10.1161/cir.0b013e3182160726.
Question 66 |
You receive an order for 40mg/kg/dose of Amoxicillin every 12 hours. Pt’s weight is 18 lbs. You have 250mg/5ml of amoxicillin suspension. Calculate the total amount in milliliters needed for 10 day supply. Round up your answer to the nearest 1.
14 mls
| |
132 mls
| |
96 mls
| |
86 mls
| |
36 mls |
Question 66 Explanation:
If 40mg of amoxicillin are needed per kg of body weight then the dose of amoxicillin is 40mg multiplied by the patient’s body weight. This patient weighs 18 lbs, based on the conversion of 2.2 lbs = 1 kg, the patient weighs 8.2 kg. 40 mg multiplied by 8.2 kg is equal to 328 mg, this is one dose of amoxicillin. If the amoxicillin comes in 250 mg/5 mL, then it needs to be determined how many mLs it will take to get 328 mg of amoxicillin. In order to do this 328 mg needs to be divided by 250 mg to get a ratio. This comes out to be 1.312. This ratio can be multiplied by the number of mLs it takes to make up 250 mg, which is 5 mLs. 1.312 multiplied by 5 mLs is 6.56 mL, this is how many mLs it will take to have 328 mg. This volume is for 1 single dose of amoxicillin. The patient is receiving 2 doses per day and for a total of 10 days, this means the patient will be receiving 20 doses. 20 doses multiplied by 6.56 mL doses equals the total volume the patient will be receiving, which is 131.2 mL.
Question 67 |
Which of the following medication may increase LDL?
Amiodarone
| |
Lisinopril
| |
Hydrochlorothiazide
| |
Acetaminophen
| |
Cyclosporine |
Question 67 Explanation:
LDL can be elevated by diuretics, cyclosporine, glucocorticoids, and amiodarone.
Reference:
Stone N, Robinson J, Lichtenstein A et al. 2013 ACC/AHA Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults. Circulation. 2013;129(25 suppl 2):S1-S45. doi:10.1161/01.cir.0000437738.63853.7a. Retrieved on Feb 6th 2017 from : http://circ.ahajournals.org/content/129/25_suppl_2/S1
Reference:
Stone N, Robinson J, Lichtenstein A et al. 2013 ACC/AHA Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults. Circulation. 2013;129(25 suppl 2):S1-S45. doi:10.1161/01.cir.0000437738.63853.7a. Retrieved on Feb 6th 2017 from : http://circ.ahajournals.org/content/129/25_suppl_2/S1
Question 68 |
Which of the following is/are nominal data?
Sex
| |
Race
| |
Blood Group
| |
NYHA stages I-IV
| |
Stages of breast cancer |
Question 68 Explanation:
Nominal data is considered unordered categories. Sex answers fall into male or female which is unordered. Race can be multiple answers such as Caucasian, African American, Asian, etc which is unordered. Blood group can only have blood type O, A, B, or AB which is also unordered. Ordered, or ordinal data would have categories that are in some sort of order
Reference:
"Statistics at Square One | The BMJ". Bmj.com. 2016. Web. 7 Nov. 2016. Available at: http://www.bmj.com/about-bmj/resources-readers/publications/statistics-square-one
Reference:
"Statistics at Square One | The BMJ". Bmj.com. 2016. Web. 7 Nov. 2016. Available at: http://www.bmj.com/about-bmj/resources-readers/publications/statistics-square-one
Question 69 |
If a patient takes 0.5mg of intravenous hydromorphone every 4hrs what would be the equivalent orals total daily dose? Hydromorphone oral to parenteral ratio 7.5:1.5.
15mg
| |
20mg
| |
10mg
| |
5mg
| |
7.5mg |
Question 69 Explanation:
To determine the dose conversion IV to PO, the ratio of PO to IV needs to be determined, this is 7.5 / 1.5 which is 5. This number means that the PO dose is 5 times more than the IV dose to get the same amount of drug into the bloodstream. If the patient is taking 0.5 mg IV then the PO dose would be 0.5 mg multiplied by 5, which is 2.5 mg. Since the patient is taking the medication every 4 hours the patient is receiving 6 doses, 24hrs/4hrs = 6. Since the patient is receiving 2.5 mg every dose and is receiving 6 doses a day, the patient is receiving 15 mg, 2.5 mg multiplied by 6 doses.
Question 70 |
Proportion of people in a population who have a particular disease at a specified point in time or over a specified period of time is definition as which of the following?
Incidence rate | |
Prevalence rate
| |
Mortality rate
| |
Relative risk
| |
Odds ratio |
Question 70 Explanation:
Incidence rate = New reported cases / summed person-years of observation (avg population during time interval)
Prevalence = Cases in a population in a given time period / total population at that time
Reference:
I. Dicker, R. C., Coronado, F., Koo, D., et al. Principals of Epidemiology in Public Health Practice, Third Edition: An Introduction to Applied Epidemiology and Biostatistics; Lesson 3, Section 2. Oct. 2006 Retrieved Jan. 24, 2017 from: https://www.cdc.gov/ophss/csels/dsepd/ss1978/lesson3/section2.html Updated: Nov. 2011
II. Numerators, denominators and populations at risk. Jun. 20, 2010. Retrieved Jan. 24, 2017 from: http://www.healthknowledge.org.uk/public-health-textbook/research-methods/1a-epidemiology/numerators-denominators-populations
Reference:
I. Dicker, R. C., Coronado, F., Koo, D., et al. Principals of Epidemiology in Public Health Practice, Third Edition: An Introduction to Applied Epidemiology and Biostatistics; Lesson 3, Section 2. Oct. 2006 Retrieved Jan. 24, 2017 from: https://www.cdc.gov/ophss/csels/dsepd/ss1978/lesson3/section2.html Updated: Nov. 2011
II. Numerators, denominators and populations at risk. Jun. 20, 2010. Retrieved Jan. 24, 2017 from: http://www.healthknowledge.org.uk/public-health-textbook/research-methods/1a-epidemiology/numerators-denominators-populations
Question 71 |
Which of the following would be most appropriate to treat infections associated with stenotrophomonas maltophilia?
Meropenem
| |
Vancomycin
| |
Ciprofloxacin
| |
Sulfamethoxazole/trimethoprim
| |
Ampicillin |
Question 71 Explanation:
Primary treatment for stenotrophomonas maltophilia is SMX-TMP. Meropenem, ciprofloxacin, Ampicillin and vancomycin have no coverage.
Reference:
Gilbert D. The Sanford Guide to Antimicrobial Therapy 2014. Sperryville, Va.: Antimicrobial Therapy; 2014
Reference:
Gilbert D. The Sanford Guide to Antimicrobial Therapy 2014. Sperryville, Va.: Antimicrobial Therapy; 2014
Question 72 |
What vitamin should the a patient receive to avoid Wernicke- Korsakoff syndrome?
Thiamine
| |
Cyanocobalamin
| |
Folic Acid
| |
Nicotinic Acid
| |
Magnesium |
Question 72 Explanation:
Thiamine should be administered to prevent Wernicke’s encephalopathy.
Reference:
Management of moderate and severe alcohol withdrawal syndromes. Uptodate.com. 2016. Available at: http://www.uptodate.com/contents/management-of-moderate-and-severe-alcohol-withdrawal-syndromes Accessed May 24, 2016.
Reference:
Management of moderate and severe alcohol withdrawal syndromes. Uptodate.com. 2016. Available at: http://www.uptodate.com/contents/management-of-moderate-and-severe-alcohol-withdrawal-syndromes Accessed May 24, 2016.
Question 73 |
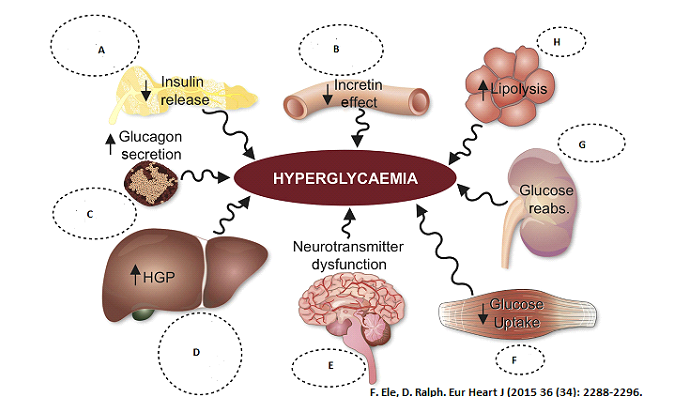 Select the class of Anti-diabetic medication that works in the specified organ to prevent hyperglycemia. Select all that applies.
Pancreases (A)
Select the class of Anti-diabetic medication that works in the specified organ to prevent hyperglycemia. Select all that applies.
Pancreases (A)Sulfonylureas | |
Alpha- Glucosidase Inhibitors | |
DPP4 Inhibitors | |
Glucagon-like peptide-1 receptor agonists | |
Thiazolidinediones | |
Biguanide | |
SGLT2 inhibitors |
Question 73 Explanation:
(A) Sulfonylureas, (C) DPP4 Inhibitors, (D) Glucagon-like peptide-1 receptor agonists
Sulfonylureas work in beta cells in the pancreas that are still functioning to enhance insulin secretion. Alpha-Glucosidase Inhibitors stop α-glucosidase enzymes in the small intestine and delay digestion and absorption of starch and disaccharides which lowers the levels of glucose after meals. DPP4 blocks the degradation ofGLP-1, GIP, and a variety of other peptides, including brain natriuretic peptide. Glucagon-like peptide-1 receptor agonists work in various organs of the body. Glucagon-like peptide-1 receptor agonists enhance glucose homeostasis through: (i) stimulation of insulin secretion; (ii) inhibition of glucagon secretion; (iii) direct and indirect suppression of endogenous glucose production; (iv) suppression of appetite; (v) enhanced insulin sensitivity secondary to weight loss; (vi) delayed gastric emptying, resulting in decreased postprandial hyperglycaemia.Thiazolidinediones are the only true insulin-sensitising agents, exerting their effects in skeletaland cardiac muscle, liver,and adipose tissue. It ameliorates insulin resistance, decreases visceral fat.Biguanides work in liver, muscle, adipose tissue via activation of AMP-activated protein kinase (AMPK) reduce hepatic glucose production. SGLT2 inhibitors work in the kidneys to inhibit sodium-glucose transport proteins to reabsorb glucose into the blood from muscle cells; overall this helps to improve insulin release from the beta cells of the pancreas.
Reference:
Reference:
- Eur Heart J (2015) 36 (34): 2288-2296. DOI: https://doi.org/10.1093.eurheart
- Ferrannini, E, DeFronzo, R. Impact of glucose-lowering drugs on cardiovascular disease in type 2 diabetes. Eur Heart J (2015) 36 (34): 2288-2296Eur Heart J (2015) 36 (34): 2288-2296. DOI: https://doi.org/10.1093/eurheartj/ehv239.
- Kennedy M, Masharani U. Pancreatic Hormones & Antidiabetic Drugs. In: Katzung BG, Trevor AJ. eds. Basic & Clinical Pharmacology, 13e New York, NY: McGraw-Hill; 2015.
- Powers AC, D'Alessio D. Endocrine Pancreas and Pharmacotherapy of Diabetes Mellitus and Hypoglycemia. In: Brunton LL, Chabner BA, Knollmann BC. eds. Goodman & Gilman's: The Pharmacological Basis of Therapeutics, 12e New York, NY: McGraw-Hill; 2015.
Question 74 |
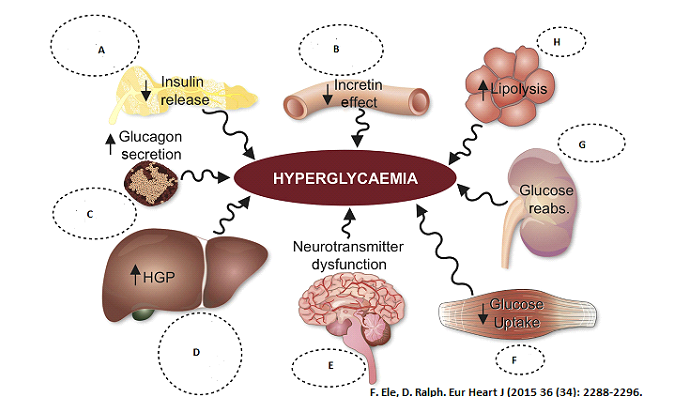 Select the class of Anti-diabetic medication that works in the specified organ to prevent hyperglycemia. Select all that applies.
GI tract (B)
Select the class of Anti-diabetic medication that works in the specified organ to prevent hyperglycemia. Select all that applies.
GI tract (B)Sulfonylureas | |
Alpha- Glucosidase Inhibitors | |
DPP4 Inhibitors | |
Glucagon-like peptide-1 receptor agonists | |
Thiazolidinediones | |
Biguanide | |
SGLT2 inhibitors |
Question 74 Explanation:
Sulfonylureas work in beta cells in the pancreas that are still functioning to enhance insulin secretion. Alpha-Glucosidase Inhibitors stop α-glucosidase enzymes in the small intestine and delay digestion and absorption of starch and disaccharides which lowers the levels of glucose after meals. DPP4 blocks the degradation ofGLP-1, GIP, and a variety of other peptides, including brain natriuretic peptide. Glucagon-like peptide-1 receptor agonists work in various organs of the body. Glucagon-like peptide-1 receptor agonists enhance glucose homeostasis through: (i) stimulation of insulin secretion; (ii) inhibition of glucagon secretion; (iii) direct and indirect suppression of endogenous glucose production; (iv) suppression of appetite; (v) enhanced insulin sensitivity secondary to weight loss; (vi) delayed gastric emptying, resulting in decreased postprandial hyperglycaemia.Thiazolidinediones are the only true insulin-sensitising agents, exerting their effects in skeletaland cardiac muscle, liver,and adipose tissue. It ameliorates insulin resistance, decreases visceral fat.Biguanides work in liver, muscle, adipose tissue via activation of AMP-activated protein kinase (AMPK) reduce hepatic glucose production. SGLT2 inhibitors work in the kidneys to inhibit sodium-glucose transport proteins to reabsorb glucose into the blood from muscle cells; overall this helps to improve insulin release from the beta cells of the pancreas.
Reference:
Reference:
- Eur Heart J (2015) 36 (34): 2288-2296. DOI: https://doi.org/10.1093.eurheart
- Ferrannini, E, DeFronzo, R. Impact of glucose-lowering drugs on cardiovascular disease in type 2 diabetes. Eur Heart J (2015) 36 (34): 2288-2296Eur Heart J (2015) 36 (34): 2288-2296. DOI: https://doi.org/10.1093/eurheartj/ehv239.
- Kennedy M, Masharani U. Pancreatic Hormones & Antidiabetic Drugs. In: Katzung BG, Trevor AJ. eds. Basic & Clinical Pharmacology, 13e New York, NY: McGraw-Hill; 2015.
- Powers AC, D'Alessio D. Endocrine Pancreas and Pharmacotherapy of Diabetes Mellitus and Hypoglycemia. In: Brunton LL, Chabner BA, Knollmann BC. eds. Goodman & Gilman's: The Pharmacological Basis of Therapeutics, 12e New York, NY: McGraw-Hill; 2015.
Question 75 |
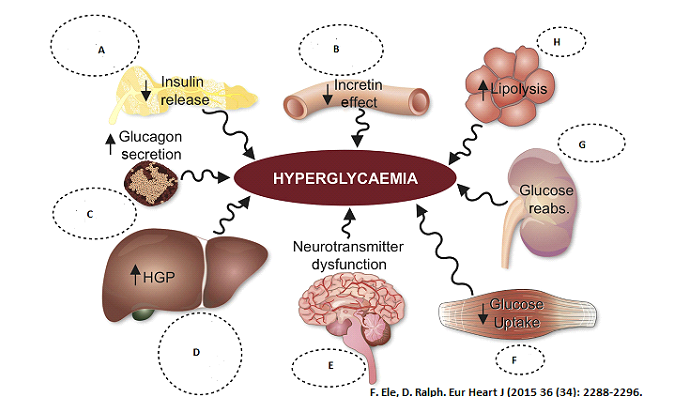 Select the class of Anti-diabetic medication that works in the specified organ to prevent hyperglycemia. Select all that applies.
Alpha cells in pancreases
Select the class of Anti-diabetic medication that works in the specified organ to prevent hyperglycemia. Select all that applies.
Alpha cells in pancreasesSulfonylureas
| |
Alpha- Glucosidase Inhibitors
| |
DPP4 Inhibitors
| |
Glucagon-like peptide-1 receptor agonists
| |
Thiazolidinediones
| |
Biguanide
| |
SGLT2 inhibitors |
Question 75 Explanation:
DPP4 Inhibitors, D Glucagon-like peptide-1 receptor agonists
Sulfonylureas work in beta cells in the pancreas that are still functioning to enhance insulin secretion. Alpha-Glucosidase Inhibitors stop α-glucosidase enzymes in the small intestine and delay digestion and absorption of starch and disaccharides which lowers the levels of glucose after meals. DPP4 blocks the degradation ofGLP-1, GIP, and a variety of other peptides, including brain natriuretic peptide. Glucagon-like peptide-1 receptor agonists work in various organs of the body. Glucagon-like peptide-1 receptor agonists enhance glucose homeostasis through: (i) stimulation of insulin secretion; (ii) inhibition of glucagon secretion; (iii) direct and indirect suppression of endogenous glucose production; (iv) suppression of appetite; (v) enhanced insulin sensitivity secondary to weight loss; (vi) delayed gastric emptying, resulting in decreased postprandial hyperglycaemia. Thiazolidinediones are the only true insulin-sensitising agents, exerting their effects in skeletal and cardiac muscle, liver, and adipose tissue. It ameliorates insulin resistance, decreases visceral fat. Biguanides work in liver, muscle, adipose tissue via activation of AMP-activated protein kinase (AMPK) reduce hepatic glucose production. SGLT2 inhibitors work in the kidneys to inhibit sodium-glucose transport proteins to reabsorb glucose into the blood from muscle cells; overall this helps to improve insulin release from the beta cells of the pancreas.
Reference:
Reference:
- Eur Heart J (2015) 36 (34): 2288-2296. DOI: https://doi.org/10.1093.eurheart
- Ferrannini, E, DeFronzo, R. Impact of glucose-lowering drugs on cardiovascular disease in type 2 diabetes. Eur Heart J (2015) 36 (34): 2288-2296Eur Heart J (2015) 36 (34): 2288-2296. DOI: https://doi.org/10.1093/eurheartj/ehv239.
- Kennedy M, Masharani U. Pancreatic Hormones & Antidiabetic Drugs. In: Katzung BG, Trevor AJ. eds. Basic & Clinical Pharmacology, 13e New York, NY: McGraw-Hill; 2015.
- Powers AC, D'Alessio D. Endocrine Pancreas and Pharmacotherapy of Diabetes Mellitus and Hypoglycemia. In: Brunton LL, Chabner BA, Knollmann BC. eds. Goodman & Gilman's: The Pharmacological Basis of Therapeutics, 12e New York, NY: McGraw-Hill; 2015.
Question 76 |
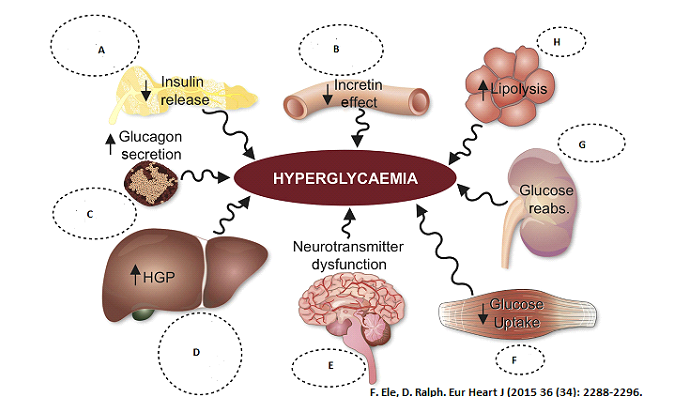 Select the class of Anti-diabetic medication that works in the specified organ to prevent hyperglycemia. Select all that applies.
Liver (D)
Select the class of Anti-diabetic medication that works in the specified organ to prevent hyperglycemia. Select all that applies.
Liver (D)Sulfonylureas
| |
Alpha- Glucosidase Inhibitors
| |
DPP4 Inhibitors
| |
Glucagon-like peptide-1 receptor agonists
| |
Thiazolidinediones
| |
Biguanide
| |
SGLT2 inhibitors |
Question 76 Explanation:
DPP4 Inhibitors, (D)Glucagon-like peptide-1 receptor agonists, (E)Thiazolidinediones (F)Biguanide
Sulfonylureas work in beta cells in the pancreas that are still functioning to enhance insulin secretion. Alpha-Glucosidase Inhibitors stop α-glucosidase enzymes in the small intestine and delay digestion and absorption of starch and disaccharides which lowers the levels of glucose after meals. DPP4 blocks the degradation ofGLP-1, GIP, and a variety of other peptides, including brain natriuretic peptide. Glucagon-like peptide-1 receptor agonists work in various organs of the body. Glucagon-like peptide-1 receptor agonists enhance glucose homeostasis through: (i) stimulation of insulin secretion; (ii) inhibition of glucagon secretion; (iii) direct and indirect suppression of endogenous glucose production; (iv) suppression of appetite; (v) enhanced insulin sensitivity secondary to weight loss; (vi) delayed gastric emptying, resulting in decreased postprandial hyperglycaemia. Thiazolidinediones are the only true insulin-sensitising agents, exerting their effects in skeletal and cardiac muscle, liver, and adipose tissue. It ameliorates insulin resistance, decreases visceral fat. Biguanides work in liver, muscle, adipose tissue via activation of AMP-activated protein kinase (AMPK) reduce hepatic glucose production. SGLT2 inhibitors work in the kidneys to inhibit sodium-glucose transport proteins to reabsorb glucose into the blood from muscle cells; overall this helps to improve insulin release from the beta cells of the pancreas.
Reference:
Reference:
- Eur Heart J (2015) 36 (34): 2288-2296. DOI: https://doi.org/10.1093.eurheart
- Ferrannini, E, DeFronzo, R. Impact of glucose-lowering drugs on cardiovascular disease in type 2 diabetes. Eur Heart J (2015) 36 (34): 2288-2296Eur Heart J (2015) 36 (34): 2288-2296. DOI: https://doi.org/10.1093/eurheartj/ehv239.
- Kennedy M, Masharani U. Pancreatic Hormones & Antidiabetic Drugs. In: Katzung BG, Trevor AJ. eds. Basic & Clinical Pharmacology, 13e New York, NY: McGraw-Hill; 2015.
- Powers AC, D'Alessio D. Endocrine Pancreas and Pharmacotherapy of Diabetes Mellitus and Hypoglycemia. In: Brunton LL, Chabner BA, Knollmann BC. eds. Goodman & Gilman's: The Pharmacological Basis of Therapeutics, 12e New York, NY: McGraw-Hill; 2015.
Question 77 |
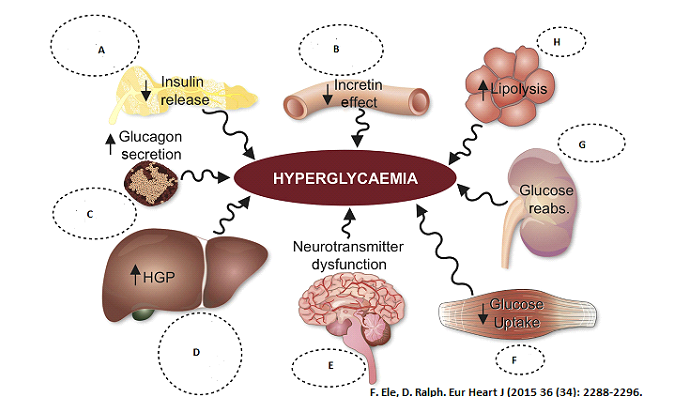 Select the class of Anti-diabetic medication that works in the specified organ to prevent hyperglycemia. Select all that applies.
Brain (E)
Select the class of Anti-diabetic medication that works in the specified organ to prevent hyperglycemia. Select all that applies.
Brain (E)Sulfonylureas
| |
Alpha- Glucosidase Inhibitors
| |
DPP4 Inhibitors
| |
Glucagon-like peptide-1 receptor agonists
| |
Thiazolidinediones
| |
Biguanide
| |
SGLT2 inhibitors |
Question 77 Explanation:
Glucagon-like peptide-1 receptor agonists
Sulfonylureas work in beta cells in the pancreas that are still functioning to enhance insulin secretion. Alpha-Glucosidase Inhibitors stop α-glucosidase enzymes in the small intestine and delay digestion and absorption of starch and disaccharides which lowers the levels of glucose after meals. DPP4 blocks the degradation ofGLP-1, GIP, and a variety of other peptides, including brain natriuretic peptide. Glucagon-like peptide-1 receptor agonists work in various organs of the body. Glucagon-like peptide-1 receptor agonists enhance glucose homeostasis through: (i) stimulation of insulin secretion; (ii) inhibition of glucagon secretion; (iii) direct and indirect suppression of endogenous glucose production; (iv) suppression of appetite; (v) enhanced insulin sensitivity secondary to weight loss; (vi) delayed gastric emptying, resulting in decreased postprandial hyperglycaemia. Thiazolidinediones are the only true insulin-sensitising agents, exerting their effects in skeletal and cardiac muscle, liver, and adipose tissue. It ameliorates insulin resistance, decreases visceral fat. Biguanides work in liver, muscle, adipose tissue via activation of AMP-activated protein kinase (AMPK) reduce hepatic glucose production. SGLT2 inhibitors work in the kidneys to inhibit sodium-glucose transport proteins to reabsorb glucose into the blood from muscle cells; overall this helps to improve insulin release from the beta cells of the pancreas.
Reference:
Reference:
- Eur Heart J (2015) 36 (34): 2288-2296. DOI: https://doi.org/10.1093.eurheart
- Ferrannini, E, DeFronzo, R. Impact of glucose-lowering drugs on cardiovascular disease in type 2 diabetes. Eur Heart J (2015) 36 (34): 2288-2296Eur Heart J (2015) 36 (34): 2288-2296. DOI: https://doi.org/10.1093/eurheartj/ehv239.
- Kennedy M, Masharani U. Pancreatic Hormones & Antidiabetic Drugs. In: Katzung BG, Trevor AJ. eds. Basic & Clinical Pharmacology, 13e New York, NY: McGraw-Hill; 2015.
- Powers AC, D'Alessio D. Endocrine Pancreas and Pharmacotherapy of Diabetes Mellitus and Hypoglycemia. In: Brunton LL, Chabner BA, Knollmann BC. eds. Goodman & Gilman's: The Pharmacological Basis of Therapeutics, 12e New York, NY: McGraw-Hill; 2015.
Question 78 |
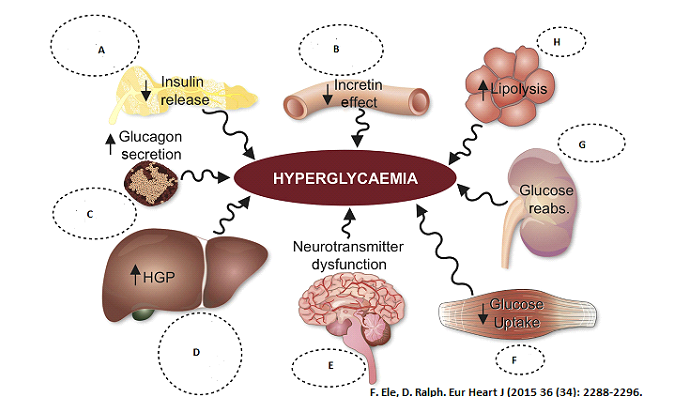 Select the class of Anti-diabetic medication that works in the specified organ to prevent hyperglycemia. Select all that applies.
Muscle (F)
Select the class of Anti-diabetic medication that works in the specified organ to prevent hyperglycemia. Select all that applies.
Muscle (F)Sulfonylureas
| |
Alpha- Glucosidase Inhibitors
| |
DPP4 Inhibitors
| |
Glucagon-like peptide-1 receptor agonists
| |
Thiazolidinediones
| |
Biguanide
| |
SGLT2 inhibitors |
Question 78 Explanation:
Sulfonylureas work in beta cells in the pancreas that are still functioning to enhance insulin secretion. Alpha-Glucosidase Inhibitors stop α-glucosidase enzymes in the small intestine and delay digestion and absorption of starch and disaccharides which lowers the levels of glucose after meals. DPP4 blocks the degradation ofGLP-1, GIP, and a variety of other peptides, including brain natriuretic peptide. Glucagon-like peptide-1 receptor agonists work in various organs of the body. Glucagon-like peptide-1 receptor agonists enhance glucose homeostasis through: (i) stimulation of insulin secretion; (ii) inhibition of glucagon secretion; (iii) direct and indirect suppression of endogenous glucose production; (iv) suppression of appetite; (v) enhanced insulin sensitivity secondary to weight loss; (vi) delayed gastric emptying, resulting in decreased postprandial hyperglycaemia. Thiazolidinediones are the only true insulin-sensitising agents, exerting their effects in skeletal and cardiac muscle, liver, and adipose tissue. It ameliorates insulin resistance, decreases visceral fat. Biguanides work in liver, muscle, adipose tissue via activation of AMP-activated protein kinase (AMPK) reduce hepatic glucose production. SGLT2 inhibitors work in the kidneys to inhibit sodium-glucose transport proteins to reabsorb glucose into the blood from muscle cells; overall this helps to improve insulin release from the beta cells of the pancreas.
Reference:
Reference:
- Eur Heart J (2015) 36 (34): 2288-2296. DOI: https://doi.org/10.1093.eurheart
- Ferrannini, E, DeFronzo, R. Impact of glucose-lowering drugs on cardiovascular disease in type 2 diabetes. Eur Heart J (2015) 36 (34): 2288-2296Eur Heart J (2015) 36 (34): 2288-2296. DOI: https://doi.org/10.1093/eurheartj/ehv239.
- Kennedy M, Masharani U. Pancreatic Hormones & Antidiabetic Drugs. In: Katzung BG, Trevor AJ. eds. Basic & Clinical Pharmacology, 13e New York, NY: McGraw-Hill; 2015.
- Powers AC, D'Alessio D. Endocrine Pancreas and Pharmacotherapy of Diabetes Mellitus and Hypoglycemia. In: Brunton LL, Chabner BA, Knollmann BC. eds. Goodman & Gilman's: The Pharmacological Basis of Therapeutics, 12e New York, NY: McGraw-Hill; 2015.
Question 79 |
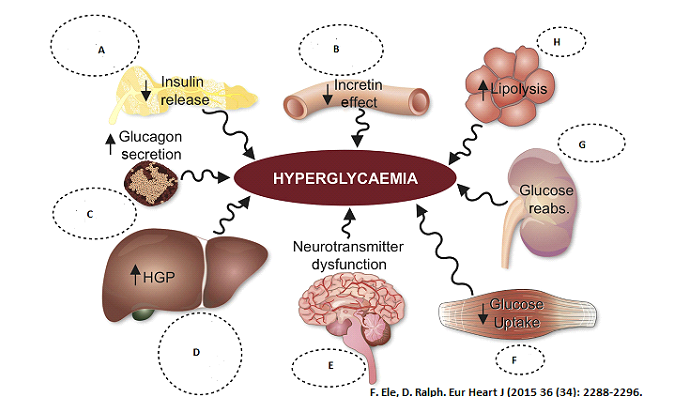 Select the class of Anti-diabetic medication that works in the specified organ to prevent hyperglycemia. Select all that applies.
Kidney (G)
Select the class of Anti-diabetic medication that works in the specified organ to prevent hyperglycemia. Select all that applies.
Kidney (G)Sulfonylureas
| |
Alpha- Glucosidase Inhibitors
| |
DPP4 Inhibitors
| |
Glucagon-like peptide-1 receptor agonists
| |
Thiazolidinediones
| |
Biguanide
| |
SGLT2 inhibitors |
Question 79 Explanation:
SGLT2 inhibitors
Sulfonylureas work in beta cells in the pancreas that are still functioning to enhance insulin secretion. Alpha-Glucosidase Inhibitors stop α-glucosidase enzymes in the small intestine and delay digestion and absorption of starch and disaccharides which lowers the levels of glucose after meals. DPP4 blocks the degradation ofGLP-1, GIP, and a variety of other peptides, including brain natriuretic peptide. Glucagon-like peptide-1 receptor agonists work in various organs of the body. Glucagon-like peptide-1 receptor agonists enhance glucose homeostasis through: (i) stimulation of insulin secretion; (ii) inhibition of glucagon secretion; (iii) direct and indirect suppression of endogenous glucose production; (iv) suppression of appetite; (v) enhanced insulin sensitivity secondary to weight loss; (vi) delayed gastric emptying, resulting in decreased postprandial hyperglycaemia. Thiazolidinediones are the only true insulin-sensitising agents, exerting their effects in skeletal and cardiac muscle, liver, and adipose tissue. It ameliorates insulin resistance, decreases visceral fat. Biguanides work in liver, muscle, adipose tissue via activation of AMP-activated protein kinase (AMPK) reduce hepatic glucose production. SGLT2 inhibitors work in the kidneys to inhibit sodium-glucose transport proteins to reabsorb glucose into the blood from muscle cells; overall this helps to improve insulin release from the beta cells of the pancreas.
Reference:
Reference:
- Eur Heart J (2015) 36 (34): 2288-2296. DOI: https://doi.org/10.1093.eurheart
- Ferrannini, E, DeFronzo, R. Impact of glucose-lowering drugs on cardiovascular disease in type 2 diabetes. Eur Heart J (2015) 36 (34): 2288-2296Eur Heart J (2015) 36 (34): 2288-2296. DOI: https://doi.org/10.1093/eurheartj/ehv239.
- Kennedy M, Masharani U. Pancreatic Hormones & Antidiabetic Drugs. In: Katzung BG, Trevor AJ. eds. Basic & Clinical Pharmacology, 13e New York, NY: McGraw-Hill; 2015.
- Powers AC, D'Alessio D. Endocrine Pancreas and Pharmacotherapy of Diabetes Mellitus and Hypoglycemia. In: Brunton LL, Chabner BA, Knollmann BC. eds. Goodman & Gilman's: The Pharmacological Basis of Therapeutics, 12e New York, NY: McGraw-Hill; 2015.
Question 80 |
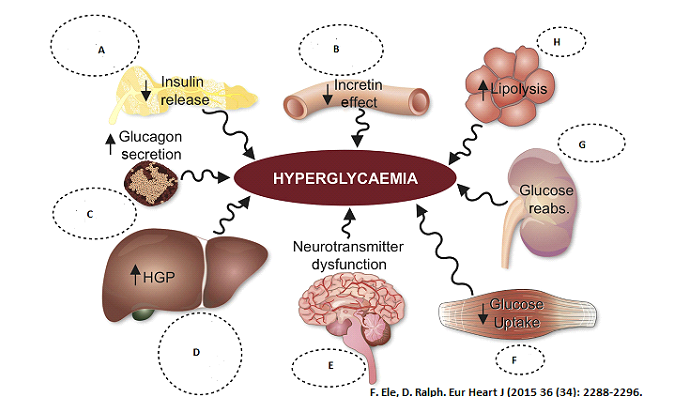 Select the class of Anti-diabetic medication that works in the specified organto prevent hyperglycemia. Select all that applies.
Fat Tissue (H)
Select the class of Anti-diabetic medication that works in the specified organto prevent hyperglycemia. Select all that applies.
Fat Tissue (H)Sulfonylureas
| |
Alpha- Glucosidase Inhibitors
| |
DPP4 Inhibitors
| |
Glucagon-like peptide-1 receptor agonists
| |
Thiazolidinediones
| |
Biguanide
| |
SGLT2 inhibitors |
Question 80 Explanation:
Thiazolidinediones
Sulfonylureas work in beta cells in the pancreas that are still functioning to enhance insulin secretion. Alpha-Glucosidase Inhibitors stop α-glucosidase enzymes in the small intestine and delay digestion and absorption of starch and disaccharides which lowers the levels of glucose after meals. DPP4 blocks the degradation ofGLP-1, GIP, and a variety of other peptides, including brain natriuretic peptide. Glucagon-like peptide-1 receptor agonists work in various organs of the body. Glucagon-like peptide-1 receptor agonists enhance glucose homeostasis through: (i) stimulation of insulin secretion; (ii) inhibition of glucagon secretion; (iii) direct and indirect suppression of endogenous glucose production; (iv) suppression of appetite; (v) enhanced insulin sensitivity secondary to weight loss; (vi) delayed gastric emptying, resulting in decreased postprandial hyperglycaemia. Thiazolidinediones are the only true insulin-sensitising agents, exerting their effects in skeletal and cardiac muscle, liver, and adipose tissue. It ameliorates insulin resistance, decreases visceral fat. Biguanides work in liver, muscle, adipose tissue via activation of AMP-activated protein kinase (AMPK) reduce hepatic glucose production. SGLT2 inhibitors work in the kidneys to inhibit sodium-glucose transport proteins to reabsorb glucose into the blood from muscle cells; overall this helps to improve insulin release from the beta cells of the pancreas.
Reference:
Reference:
- Eur Heart J (2015) 36 (34): 2288-2296. DOI: https://doi.org/10.1093.eurheart
- Ferrannini, E, DeFronzo, R. Impact of glucose-lowering drugs on cardiovascular disease in type 2 diabetes. Eur Heart J (2015) 36 (34): 2288-2296Eur Heart J (2015) 36 (34): 2288-2296. DOI: https://doi.org/10.1093/eurheartj/ehv239.
- Kennedy M, Masharani U. Pancreatic Hormones & Antidiabetic Drugs. In: Katzung BG, Trevor AJ. eds. Basic & Clinical Pharmacology, 13e New York, NY: McGraw-Hill; 2015.
- Powers AC, D'Alessio D. Endocrine Pancreas and Pharmacotherapy of Diabetes Mellitus and Hypoglycemia. In: Brunton LL, Chabner BA, Knollmann BC. eds. Goodman & Gilman's: The Pharmacological Basis of Therapeutics, 12e New York, NY: McGraw-Hill; 2015.
Question 81 |
LT is a 42 year old white female with past medical history of epilepsy, gastroesophageal reflux disease and seasonal allergies. She weighs 86 kg, height 5’6” and allergic to Aspirin (rash) and Phenobarbital (difficulty breathing). Her medications includes Omeprazole 40mg daily, Phenytoin 200mg twice daily, Valproic acid 500mg four times daily, Loratadine 10mg daily. She comes to your community pharmacy to pick up prescription for Primidone 250mg twice daily.
Pertaining to Primidone what is the most appropriate action to take?
Notify the physician, Primidone dose is too low. | |
Notify the physician, Primidone in contraindicated in patient with phenobarbital allergy.
| |
Notify the physician, Primidone in contraindicated in patient with Aspirin allergy.
| |
Notify the physician, patient is already on three anti-seizure medication and primidone is not needed.
| |
Notify the physician, Primidone in contraindicated in patient with gastroesophageal reflux disease. |
Question 81 Explanation:
Primidone is an anticonvulsant drug that is structurally related to phenobarbital. Primidone is metabolized to phenobarbital and therefore shares its anticonvulsant and sedative properties. Primidone may be more effective than therapy with phenobarbital alone because primidone and both of its metabolites, phenobarbital and phenylethylmalonamide (PEMA), possess anticonvulsant activity.
Reference:
Mysoline (primidone) package insert. Bridgewater, NJ: Valeant Pharmaceuticals, LLC; 2016 Nov.
Reference:
Mysoline (primidone) package insert. Bridgewater, NJ: Valeant Pharmaceuticals, LLC; 2016 Nov.
Question 82 |
After talking to the physician you find out her labs. Her labs reveled albumin level of 2.1gm/dL, calcium of 7.8mg/dL, glucose 120mg/dL , sodium 138 mmol/L, phenytoin level of 17.8. Based on the given data which of the following best interprets phenytoin concentration?
Phenytoin level is with normal limits
| |
Phenytoin level is too high
| |
Phenytoin level is too low
| |
Phenytoin level cannot be determined
| |
Phenytoin level need to be repeated |
Question 82 Explanation:
Corrected phenytoin (mg/L) = Observed phenytoin (mg/L) /(0.2 x albumin [g/dL]) + 0.1
= 17.8/(0.2 x 2.1)+ 0.1
= 17.8/0.42 + 0.1
= 42.48mg/L ← phenytoin level is high.
Normal therapeutic range is: 10-20mg/dL
Reference:
Von Winckelmann SL, Spret I, Willems L. Therapeutic drug monitoring of phenytoin in critically ill patients. Pharmacotherapy 2008;28(11):1391–400.
= 17.8/(0.2 x 2.1)+ 0.1
= 17.8/0.42 + 0.1
= 42.48mg/L ← phenytoin level is high.
Normal therapeutic range is: 10-20mg/dL
Reference:
Von Winckelmann SL, Spret I, Willems L. Therapeutic drug monitoring of phenytoin in critically ill patients. Pharmacotherapy 2008;28(11):1391–400.
Question 83 |
After talking to the patient you find out LT has been incompliant with her three times a day Valproic acid, level came back at 35 mmol/L. What is the most appropriate course of action?
Notify the physician to decrease the dose of Valproic acid.
| |
Notify the physician to increse the dose of Valproic acid.
| |
Albumin needs to be obtained to calculate corrected Valproic acid level
| |
Valproic acid level is within normal limit, no adjustment is needed. | |
Valproic acid level is within normal limit, no adjustment is needed |
Question 83 Explanation:
The delayed-release action of divalproex allows for less frequent dosing than valproic acid in some patients. Divalproex sodium contains sodium valproate and valproic acid in a 1:1 molar stable co-ordination compound. Valproic acid, sodium valproate, and divalproex share the same pharmacology; however, there are pharmacokinetic differences among products.
Reference:
Depakote (divalproex sodium tablets) package insert. North Chicago, IL: AbbVie Inc.; 2016 Nov.
Reference:
Depakote (divalproex sodium tablets) package insert. North Chicago, IL: AbbVie Inc.; 2016 Nov.
Question 84 |
Which of the following is recommended to be monitored in patients on Divalproex Sodium?
CBC
| |
Serum ammonia
| |
LFT’s
| |
Pulmonary function
| |
Serum creatinine |
Question 84 Explanation:
A, B, C. Hepatotoxicity, including hepatic failure, has been fatal and may more commonly occur in the first 6 months of treatment. Valproic acid and its analogs are contraindicated in patients with known urea cycle disorders. Patients with urea cycle disorders have a genetic enzyme defect leading to an impaired ability to produce urea. Hyperammonemic encephalopathy has been reported following initiation of valproate therapy. Because of, inhibition of the secondary phase of platelet aggregation, and abnormal coagulation parameters complete blood counts and coagulation tests are recommended before initiating valproic acid therapy and at periodic intervals.
Reference:
Depacon (valproate sodium injection) package insert. North Chicago, IL: Abbvie Inc.; 2017 April.
Reference:
Depacon (valproate sodium injection) package insert. North Chicago, IL: Abbvie Inc.; 2017 April.
Question 85 |
An order is received for 0.03 units /min of vasopressin for Sepsis to maintain MAP >65. The standard mixed in your hospital for vasopressin is 40 units in 100ml NS. What is the rate in mLs/hr should the vasopressin be infused at?
4.0 ml/hr
| |
4.9ml/hr
| |
4.5ml/hr
| |
3.5ml/hr
| |
6ml/hr |
Question 85 Explanation:
Rate of infusion: 100mL/40U x 0.03U/min x 60min/1 hr = 4.5mL/hr
Question 86 |
Which of the following Anti-epileptic medication can cause pancreatitis?
Carbamazepine
| |
Gabapentin
| |
Valproic acid
| |
Levetiracetam
| |
Phenobarbital |
Question 86 Explanation:
Cases of life-threatening pancreatitis have been reported in both pediatric and adult patients receiving valproic acid or its analogs. Patients should be warned that abdominal pain, nausea, vomiting, and/or anorexia can be symptoms of pancreatitis that require prompt medical evaluation. If pancreatitis is diagnosed, valproate should be discontinued.
Reference:
Clinical Pharmacology, Available at: http://www.clinicalpharmacology-ip.com/Forms/Monograph/monograph.aspx?cpnum=637&sec=moncontr&t=0 Accessed May 2017
Reference:
Clinical Pharmacology, Available at: http://www.clinicalpharmacology-ip.com/Forms/Monograph/monograph.aspx?cpnum=637&sec=moncontr&t=0 Accessed May 2017
Question 87 |
Which of the following side effects should LT be made aware of while on Divalproex Sodium?
Weight gain
| |
Oligomenorrhea
| |
Alopecia
| |
Gynecomastia
| |
Gingival hyperplasia |
Question 87 Explanation:
Common GI side effects of Valproic Acid and Divalproex Sodium are Weight gain, Nausea, Vomiting, Diarrhea, abdominal pain, dyspepsia. Divalproex sodium or valproic acid affects reproductive endocrine function in women. Menstrual irregularities defined as amenorrhea, oligomenorrhea, and prolonged cycles were common. Gynecomastia is not a side effect of Divalproex Sodium. For list of drugs that causes gynecomastia refer the reference. Gingival hyperplasia is a well-known side effect of phenytoin.
Reference: Depakote (divalproex sodium tablets) package insert. North Chicago, IL: AbbVie Inc.; 2017 May. Drug-induced gynecomastia. Giuseppe R, Mauro M. Available at: http://www.pharmaco-vigilance.eu/content/drug-induced-gynecomastia . Accessed May 2017
Reference: Depakote (divalproex sodium tablets) package insert. North Chicago, IL: AbbVie Inc.; 2017 May. Drug-induced gynecomastia. Giuseppe R, Mauro M. Available at: http://www.pharmaco-vigilance.eu/content/drug-induced-gynecomastia . Accessed May 2017
Question 88 |
What indication usually requires higher dose of proton pump inhibitor?
Helicobacter pylori
| |
Esophagitis
| |
Duodenal ulcer
| |
Stress ulcer prophylaxis
| |
Zollinger-Ellison syndrome |
Question 88 Explanation:
The diagnosis of Zollinger-Ellison syndrome is suggested when plasma gastrin is > 1000 pg/ml and the basal acid output is > 15 mEq/h or when associated with a pH < 2. The treatment is focused on controlling gastric acid hypersecretion and localisation of the tumour and its metastases. Proton pump inhibitors are the most effective antisecretory drugs and can be administered at high dosages
Reference:
I. Tomassetti P, Campana D. Treatment of Zollinger-Ellison Syndrome. World J Gastroenterol 2005 Sep 21; 11(35): 5423–5432.
II. Jensen RT, Gardner JD, Raufman JP, Pandol SJ, Doppman JL, Collen MJ. Zollinger-Ellison syndrome: current concepts and management. Ann Intern Med. 1983;98:59–75
Reference:
I. Tomassetti P, Campana D. Treatment of Zollinger-Ellison Syndrome. World J Gastroenterol 2005 Sep 21; 11(35): 5423–5432.
II. Jensen RT, Gardner JD, Raufman JP, Pandol SJ, Doppman JL, Collen MJ. Zollinger-Ellison syndrome: current concepts and management. Ann Intern Med. 1983;98:59–75
Question 89 |
Which of the following are complication associated with long term use of proton pump inhibitors?
Bone fractures
| |
Hypomagnesemia
| |
Vitamin B12 deficiency
| |
Clostridium difficile infection
| |
Helicobacter pylori infection |
Question 89 Explanation:
Use proton pump inhibitors (PPIs) in patients with or who have risk factors for osteoporosis cautiously. PPIs have been associated with a possible increased risk of bone fractures of the hip, wrist, and spine. Daily treatment with a gastric acid-suppressing medication over a long period of time may lead to hypomagnesemia. Vitamin B12 deficiency has been reported with long term use of PPIs in the literatures. The use of PPIs, may increase the risk of enteric infection by encouraging the growth of gut microflora and increasing susceptibility to organism including Clostridium Difficile. There are recent FDA warnings regarding C. Diff infection with use of PPIs. H. Pylori infection is not a complication of PPIs. PPIs in combination with certain antibiotics are used to treat H. pylori Infections.
Reference:
I. Targownik LE, Lix LM, Metge CJ, et al. Use of proton pump inhibitors and risk of osteoporosis-related fractures. CMAJ 2008;179:319—26.
II. Howden CW. Vitamin B12 levels during prolonged treatment with proton pump inhibitors. J Clin Gastroenterol. 2000;30:29–33.
III. Haag S, Andrews JM, Katelaris PH, et al. Management of reflux symptoms with over-the-counter proton pump inhibitors: issues and proposed guidelines. Digestion 2009;80:226-34.
Reference:
I. Targownik LE, Lix LM, Metge CJ, et al. Use of proton pump inhibitors and risk of osteoporosis-related fractures. CMAJ 2008;179:319—26.
II. Howden CW. Vitamin B12 levels during prolonged treatment with proton pump inhibitors. J Clin Gastroenterol. 2000;30:29–33.
III. Haag S, Andrews JM, Katelaris PH, et al. Management of reflux symptoms with over-the-counter proton pump inhibitors: issues and proposed guidelines. Digestion 2009;80:226-34.
Question 90 |
Concomitant use of warfarin and omeprazole is associated with increased INR and prothrombin time(PT). What enzyme dose the omeprazole inhibits that is metabolized by warfarin?
CYP3A4
| |
CYP2C9
| |
CYP2C19
| |
CYP2D9
| |
CYP1A2 |
Question 90 Explanation:
Omeprazole is CYP2C19 inhibitor which can prolong the elimination of warfarin, particularly R-warfarin. R-warfarin is partially metabolized by CYP2C19. The combined use of omeprazole and warfarin has been associated with reports of increased INR and prothrombin time (PT).
Reference:
Prilosec (omeprazole) package insert. Wilmington, DE: AstraZeneca; 2016 Dec.
Reference:
Prilosec (omeprazole) package insert. Wilmington, DE: AstraZeneca; 2016 Dec.
Question 91 |
Which of the following are non-pharmacological measure that may control symptoms of gastroesophageal reflux disease?
Remain upright after a meal
| |
Increase fat intake to reduce gastric emptying time
Reduce intake of food or beverage that may reduce | |
lower esophageal sphincter tone
| |
Wear tight fitted cloths to increase intra-abdominal pressure.
| |
Discontinue nicotine use in patients that uses tobacco product. |
Question 91 Explanation:
Non-pharmacological measure that may control symptoms of gastroesophageal reflux disease are: Avoid aggravating foods/beverages that may reduce LES pressure alcohol, citrus juices caffeine, garlic, onions or cause direct irritation such as spicy foods or tomato juice should be avoided. Reduce fat intake, remain upright after meals, avoid meal before bedtime. Avoid tight fitted cloths, decrease intra-abdominal pressure. Discontinue nicotine use. Reduce intake of food or beverage that may reduce lower esophageal sphincter tone.
Reference:
American Gastroenterological Association Institute. Medical position statement on the management of gastroesophageal reflux disease. Gastroenterology 2008;135:1383-91.
Reference:
American Gastroenterological Association Institute. Medical position statement on the management of gastroesophageal reflux disease. Gastroenterology 2008;135:1383-91.
Question 92 |
A physician needs your help to calculate the protamine dose on a patient who started hemorrhaging while on heparin. Patient has been receiving heparin at a dose of 13mls /hr for 2 hrs when the physician decides to use protamine to reverse the heparin. Heparin bag says concentration of 50 units/ml. The half-life of heparin is 60 minutes. 1 mg of protamine reverses 100 units of heparin. How much protamine should be given to this patient?
5mg
| |
10mg
| |
7mg
| |
13mg
| |
9.7mg |
Question 92 Explanation:
1st hour
13mL/hr x 1 hr= 13mL
50U/mL=XU/13mL 650U Heparin given in hours
since the half life of protamine is 60min
2nd hour 650/2 =325 units
650 units + 325 units =975 units needs to be reveresed
**1mg of protamine reverses 100U of Heparin
(1mg protamine/100U Heparin) = (Xmg protamine/975U Heparin given)
= x = 9.7mg protamine
13mL/hr x 1 hr= 13mL
50U/mL=XU/13mL 650U Heparin given in hours
since the half life of protamine is 60min
2nd hour 650/2 =325 units
650 units + 325 units =975 units needs to be reveresed
**1mg of protamine reverses 100U of Heparin
(1mg protamine/100U Heparin) = (Xmg protamine/975U Heparin given)
= x = 9.7mg protamine
Question 93 |
In a study where Rivaroxaban was compared to Enoxaparin to find total VTE following HIP replacement surgery, there were 17 total VTE out of 1513 patients in the Rivaraoaban group and 57 total VTE out of 1473 patient in the enoxaparin group. What is the absolute risk reduction of using Rivaroxaban over Enoxaparin?
17
| |
57
| |
71 | |
2.7
| |
0.27 |
Question 93 Explanation:
Absolute risk reduction: 0.027 = 2.7%
(Event rate in enoxaparin group) – (Event rate in rivaroxaban group) = (57/1473) – (17/1513) = 0.02746
Reference:
Barratt A, Wyer PC, Hatala R, et al. Tips for learners of evidence-based medicine: 1. Relative risk reduction, absolute risk reduction and number needed to treat. CMAJ. 2004;171(4):353-8. doi: 10.1503/cmaj.1021197.
(Event rate in enoxaparin group) – (Event rate in rivaroxaban group) = (57/1473) – (17/1513) = 0.02746
Reference:
Barratt A, Wyer PC, Hatala R, et al. Tips for learners of evidence-based medicine: 1. Relative risk reduction, absolute risk reduction and number needed to treat. CMAJ. 2004;171(4):353-8. doi: 10.1503/cmaj.1021197.
Question 94 |
According to the 2013 ACC/AHA Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults, which of the following medications and dosing regimens is considered moderate-intensity statin therapy?
Atorvastatin 80 mg PO QHS
| |
Lovastatin 20 mg PO QHS
| |
Simvastatin 40 mg PO QHS
| |
Rosuvastatin 40 mg PO QHS
| |
Atorvastatin 20mg PO QHS |
Question 94 Explanation:
Moderate-Intensity Statin Therapy:
Atorvastatin 10 (20) mg, Rosuvastatin (5) 10 mg, Simvastatin 20–40 mg, Pravastatin 40 (80) mg, Lovastatin 40 mg, Fluvastatin XL 80 mg, Fluvastatin 40 mg bid, Pitavastatin 2–4 mg
Reference:
Stone N, Robinson J, Lichtenstein A et al. 2013 ACC/AHA Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults. Circulation. 2013;129(25 suppl 2):S1-S45. doi:10.1161/01.cir.0000437738.63853.7a.
Reference:
Stone N, Robinson J, Lichtenstein A et al. 2013 ACC/AHA Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults. Circulation. 2013;129(25 suppl 2):S1-S45. doi:10.1161/01.cir.0000437738.63853.7a.
Question 95 |
JT is a 58 year old women who is on vancomycin empirically for pyomyositis confirmed by MRI. Surgical debridement has successfully removed infected tissue and pus. C&S of the infected tissue comes back MSSA sensitive to everything on the panel. JT is allergic to PCN (rash), she has had cephalosporin for her UTI in the past with no problem. What would be the most appropriate antibiotics to switch to while JT is still in the hospital?
Oxacillin
| |
Doxycycline
| |
Ceftaroline
| |
Daptomycin
| |
Cefazolin |
Question 95 Explanation:
Cefazolin or an antistaphylococcal penicillin (oxacillin or nafcillin) is recommended for this patient because the C&S results indicate MSSA. Since the patient develops a rash to penicillins, it would be acceptable to use cefazolin in this case.
.
Reference: Stevens, Dennis L., et al. "Practice guidelines for the diagnosis and management of skin and soft tissue infections: 2014 update by the Infectious Diseases Society of America." Clinical Infectious Diseases (2014): ciu296. Available at: https://academic.oup.com/cid/article/59/2/e10/2895845/Practice-Guidelines-for-the-Diagnosis-and
Reference: Stevens, Dennis L., et al. "Practice guidelines for the diagnosis and management of skin and soft tissue infections: 2014 update by the Infectious Diseases Society of America." Clinical Infectious Diseases (2014): ciu296. Available at: https://academic.oup.com/cid/article/59/2/e10/2895845/Practice-Guidelines-for-the-Diagnosis-and
Question 96 |
Calculate the Osmolarity of 3% hypertonic saline?
1026 mOsmol/L
| |
76.9mOsmol/L
| |
287 mOsm/L
| |
565 mOsm/L
| |
327 mOsm/L |
Question 96 Explanation:
Osmolarity = mOsmol/L = (wt of substance (g/mL))/(MW(g/mol)) x (# of particles) x 1000
Weight of substance: 3% = (3g/100mL) = (xg/1000mL) = x = 30g/L
# of particles NaCL Na+ + Cl- (2 particles) mOsmol/L = (30g/L)/(58.5g/mol) x 2 x 1000 = 1,025.6
1026 mOsmol/L
Weight of substance: 3% = (3g/100mL) = (xg/1000mL) = x = 30g/L
# of particles NaCL Na+ + Cl- (2 particles) mOsmol/L = (30g/L)/(58.5g/mol) x 2 x 1000 = 1,025.6
1026 mOsmol/L
Question 97 |
Which of the following would be most appropriate to treat stenotrophomonas maltophilia?
Meropenem
| |
Vancomycin
| |
Ciprofloxacin
| |
Sulfamethoxazole/trimethoprim
| |
Cefepime |
Question 97 Explanation:
Primary treatment for stenotrophomonas maltophilia is SMX-TMP. Meropenem, ciprofloxacin, and vancomycin have no coverage.
Reference:
Gilbert D. The Sanford Guide to Antimicrobial Therapy 2014. Sperryville, Va.: Antimicrobial Therapy; 2014
Reference:
Gilbert D. The Sanford Guide to Antimicrobial Therapy 2014. Sperryville, Va.: Antimicrobial Therapy; 2014
Question 98 |
An order is received to start Milrinone at 0.75mcg/kg/min, Milrinone comes as 20mg/100ml D5W. What is the infusion rate in mL/hr? Patient weighs 115kg.
86 mls/hr
| |
13 mls/hr | |
25.9 mls/hr
| |
43 mls/hr
| |
7 mls/hr |
Question 98 Explanation:
*Patient dose: 0.75mcg x 115kg = 86.25mcg/min
(100mL/20mg) x (86.25mcg/1hr) x (60min/1hr) x (1mg/1000mcg)
= 25.875mL/hr Rate of infusion of Milrinone
(100mL/20mg) x (86.25mcg/1hr) x (60min/1hr) x (1mg/1000mcg)
= 25.875mL/hr Rate of infusion of Milrinone
Question 99 |
MT is 47 year old man who presents to the ER with painful, red, swollen area on his left leg. His temperature is 38.4, respiratory rate 30 and heart rate 95. He has been taking cephalexin day 4 today, as prescribed by his primary care physician. His CMP is normal a CBC shows elevated WBC of 16,000/mm3. What would be the most appropriate antibiotic/s to initiate on MT empirically?
Vancomycin IV and Piperacillin/Tazobactam
| |
IV Doxycycline and Ceftazidime
| |
Nafcillin
| |
Vancomycin IV.
| |
Ceftriaxone |
Question 99 Explanation:
This patient is displaying signs of a severe case of cellulitis. Severe cellulitis is defined as having one of the following: failed oral antibiotic treatment, immunocompromised, clinical signs of deeper infection, or meeting the SIRS criteria. Based on this patient’s presentation they have failed antibiotic treatment and meet SIRS criteria. For severe cellulitis, IDSA SSTI guidelines recommend using Vancomycin along with Zosyn.
Reference:
Stevens, Dennis L., et al. "Practice guidelines for the diagnosis and management of skin and soft tissue infections: 2014 update by the Infectious Diseases Society of America." Clinical Infectious Diseases (2014): ciu296. Available at: https://academic.oup.com/cid/article/59/2/e10/2895845/Practice-Guidelines-for-the-Diagnosis-and
Reference:
Stevens, Dennis L., et al. "Practice guidelines for the diagnosis and management of skin and soft tissue infections: 2014 update by the Infectious Diseases Society of America." Clinical Infectious Diseases (2014): ciu296. Available at: https://academic.oup.com/cid/article/59/2/e10/2895845/Practice-Guidelines-for-the-Diagnosis-and
Question 100 |
If a patient takes 0.5mg of intravenous hydromorphone every 4hrs what would be the equivalent orals total daily dose? Hydromorphone oral to parenteral ratio 7.5:1.5.
15mg
| |
20mg
| |
10mg
| |
5mg
| |
7.5mg |
Question 100 Explanation:
To determine the dose conversion IV to PO, the ratio of PO to IV needs to be determined, this is 7.5 / 1.5 which is 5. This number means that the PO dose is 5 times more than the IV dose to get the same amount of drug into the bloodstream. If the patient is taking 0.5 mg IV then the PO dose would be 0.5 mg multiplied by 5, which is 2.5 mg. Since the patient is taking the medication every 4 hours the patient is receiving 6 doses, 24hrs/4hrs = 6. Since the patient is receiving 2.5 mg every dose and is receiving 6 doses a day, the patient is receiving 15 mg, 2.5 mg multiplied by 6 doses.
Once you are finished, click the button below. Any items you have not completed will be marked incorrect.
There are 100 questions to complete.
|
List |

Comments are closed.