CGP
- Cardiovascular
- Endocrine
- Geriatrics
- Gastrointestinal disorder
- Infectious disease
- Men’s and women’s health
- Neurology
- Oncology
- Ophthalmic and otic
- Pain management
- Psychiatric
- Renal disease / fluids & electrolytes
- Respiratory
- Skin conditions
- Pharmacokinetics/Pharmacodynamics
- Biostatistics and Pharmacoeconomic
- Pharmacy policy, procedure and regulations
The questions in this section are intended to test your knowledge and skills on Geriatric Pharmacy including biostatistics for practicing pharmacist and pharmacist preparing for CGP (Board Certified Geriatric Pharmacist).
Click on the right arrow to go to the next question. If the arrow is missing hover your mouse to the lower right, above the ad until the mouse is clickable.
CGP Practice Questions
Congratulations - you have completed CGP Practice Questions.
You scored %%SCORE%% out of %%TOTAL%%.
Your performance has been rated as %%RATING%%
Your answers are highlighted below.
Question 1 |
Which of the following cardiovascular changes is/are seen as body ages?
Increase in total peripheral resistance | |
Increase in cardiac output | |
Increase in baroreceptor sensitivity | |
Increase in Beta-adrenergic receptor sensitivity |
Question 1 Explanation:
Answer A. With aging, blood pressure and total peripheral resistance increase, however, a decrease in cardiac output is seen. A progressive decline in baroreceptor sensitivity is a characteristic feature of human aging as is a decrease in Beta-adrenergic receptor sensitivity.
Reference:
1. Martin WH 3rd e. Effects of aging, gender, and physical training on peripheral vascular function. - PubMed - NCBI. Ncbinlmnihgov. 2016. Available at: https://www.ncbi.nlm.nih.gov/pubmed/1860209. Accessed October 12, 2016.
2. O'Mahony D e. Reduced baroreflex sensitivity in elderly humans is not due to efferent autonomic dysfunction. - PubMed - NCBI. Ncbinlmnihgov. 2016. Available at: https://www.ncbi.nlm.nih.gov/pubmed/10600664. Accessed October 12, 2016.
3. Ferrara N, Komici K, Corbi G et al. β-adrenergic receptor responsiveness in aging heart and clinical implications. Frontiers in Physiology. 2014;4. doi:10.3389/fphys.2013.00396.
Reference:
1. Martin WH 3rd e. Effects of aging, gender, and physical training on peripheral vascular function. - PubMed - NCBI. Ncbinlmnihgov. 2016. Available at: https://www.ncbi.nlm.nih.gov/pubmed/1860209. Accessed October 12, 2016.
2. O'Mahony D e. Reduced baroreflex sensitivity in elderly humans is not due to efferent autonomic dysfunction. - PubMed - NCBI. Ncbinlmnihgov. 2016. Available at: https://www.ncbi.nlm.nih.gov/pubmed/10600664. Accessed October 12, 2016.
3. Ferrara N, Komici K, Corbi G et al. β-adrenergic receptor responsiveness in aging heart and clinical implications. Frontiers in Physiology. 2014;4. doi:10.3389/fphys.2013.00396.
Question 2 |
According to the AGS updated Beers Criteria for Potentially Inappropriate Medication Use in Older Adults which of the following statement is true regarding anti-infective agent Nitrofurantoin?
Use of Nitrofurantoin is not recommended in older adult. | |
Use of Nitrofurantoin is not recommended in older adult with creatinine clearance <60ml/min. | |
Use of Nitrofurantoin is not recommended in older adult with creatinine clearance <30ml/min. | |
Use of Nitrofurantoin is now recommended for all older adult regardless of their renal function. |
Question 2 Explanation:
The recommendation to avoid Nitrofurantoin in patients with a CrCl< 60 mL/min was revised with the 2015 update. There is evidence that it can be used in patients with a CrCl of 30 mL/min or higher for short duration.
Reference:
American Geriatrics Society 2015 Updated Beers Criteria for Potentially Inappropriate Medication Use in Older Adults. Journal of the American Geriatrics Society. 2015;63(11):2227-2246. doi:10.1111/jgs.13702.
Reference:
American Geriatrics Society 2015 Updated Beers Criteria for Potentially Inappropriate Medication Use in Older Adults. Journal of the American Geriatrics Society. 2015;63(11):2227-2246. doi:10.1111/jgs.13702.
Question 3 |
According to the AGS updated Beers Criteria for Potentially Inappropriate Medication Use in Older Adults which of the following antihypertensive medications should be avoided in older adults?
Doxazosin | |
Nifedipine immediate release | |
A and B | |
Hydrochlorothiazide |
Question 3 Explanation:
Doxazosin is a peripheral alpha blocker, which is considered a potentially inappropriate medication (PIM) in the elderly. Nifedipine IR is also listed on the Beers Criteria to be avoided in the elderly.
Reference:
American Geriatrics Society 2015 Updated Beers Criteria for Potentially Inappropriate Medication Use in Older Adults. Journal of the American Geriatrics Society. 2015;63(11):2227-2246. doi:10.1111/jgs.13702.
Reference:
American Geriatrics Society 2015 Updated Beers Criteria for Potentially Inappropriate Medication Use in Older Adults. Journal of the American Geriatrics Society. 2015;63(11):2227-2246. doi:10.1111/jgs.13702.
Question 4 |
Which of the following medications can lower patient's seizure threshold?
Bupropion | |
Tramadol | |
Olanzapine | |
All of the above can lower seizure threshold |
Question 4 Explanation:
Seizure threshold can be lowered by Bupropion, Chlorpromazine, Clozapine, Maprotiline, Olanzapine, Thioridazine, Thiothixene, and Tramadol.
Reference:
American Geriatrics Society 2015 Updated Beers Criteria for Potentially Inappropriate Medication Use in Older Adults. Journal of the American Geriatrics Society. 2015;63(11):2227-2246. doi:10.1111/jgs.13702.
Reference:
American Geriatrics Society 2015 Updated Beers Criteria for Potentially Inappropriate Medication Use in Older Adults. Journal of the American Geriatrics Society. 2015;63(11):2227-2246. doi:10.1111/jgs.13702.
Question 5 |
Which of the following pulmonary changes is/are seen as the body ages?
Decrease in expiratory flow rate | |
Decrease in vital capacity
| |
Decrease in respiratory muscle strength
| |
All of the above changes are seen a body ages
|
Question 5 Explanation:
Expiratory flow rates decrease with aging and typically show changes in the flow-volume curves. Other age-related changes that occur in the lungs include weakening of the respiratory muscles as well as a decrease in lung measures of lung function such as vital capacity, which is the maximum amount of air that can be breathed out following a maximum inhalation.
Reference:
I. Janssens J, Pache J, Nicod L. Physiological changes in respiratory function associated with ageing. European Respiratory Journal. 1999;13(1):197-205. Available at: http://erj.ersjournals.com/content/13/1/197.long. Accessed October 13, 2016.
II. System E. Effects of Aging on the Respiratory System. Merck Manuals Consumer Version. 2016. Available at: https://www.merckmanuals.com/home/lung-and-airway-disorders/biology-of-the-lungs-and-airways/effects-of-aging-on-the-respiratory-system. Accessed October 13, 2016.
Reference:
I. Janssens J, Pache J, Nicod L. Physiological changes in respiratory function associated with ageing. European Respiratory Journal. 1999;13(1):197-205. Available at: http://erj.ersjournals.com/content/13/1/197.long. Accessed October 13, 2016.
II. System E. Effects of Aging on the Respiratory System. Merck Manuals Consumer Version. 2016. Available at: https://www.merckmanuals.com/home/lung-and-airway-disorders/biology-of-the-lungs-and-airways/effects-of-aging-on-the-respiratory-system. Accessed October 13, 2016.
Question 6 |
Which of the following medications should be avoided for constipation in elderly patients?
Oral Mineral oil | |
Oral Senokot | |
Oral Docusate | |
All of the above |
Question 6 Explanation:
Mineral oil should not be administered orally in the elderly due to the risk of aspiration. There are safer alternatives.
Reference: I. American Geriatrics Society 2015 Updated Beers Criteria for Potentially Inappropriate Medication Use in Older Adults. Journal of the American Geriatrics Society. 2015;63(11):2227-2246. doi:10.1111/jgs.13702
Reference: I. American Geriatrics Society 2015 Updated Beers Criteria for Potentially Inappropriate Medication Use in Older Adults. Journal of the American Geriatrics Society. 2015;63(11):2227-2246. doi:10.1111/jgs.13702
Question 7 |
Which of the following medications should be avoided if a patient is on lithium to avoid lithium toxicity?
Lisinopril | |
Furosemide | |
A and B | |
Metoprolol |
Question 7 Explanation:
ACE-inhibitors (such as lisinopril) and loop diuretics (furosemide) can both increase the risk of lithium toxicity.
Reference:
American Geriatrics Society 2015 Updated Beers Criteria for Potentially Inappropriate Medication Use in Older Adults. Journal of the American Geriatrics Society. 2015;63(11):2227-2246. doi:10.1111/jgs.13702.
Reference:
American Geriatrics Society 2015 Updated Beers Criteria for Potentially Inappropriate Medication Use in Older Adults. Journal of the American Geriatrics Society. 2015;63(11):2227-2246. doi:10.1111/jgs.13702.
Question 8 |
Which of the following medications should be avoided with warfarin?
Amiodarone | |
Lithium | |
Amiloride | |
Enalapril |
Question 8 Explanation:
Amiodarone and NSAIDs can both interact with warfarin causing an increased risk of bleeding. Amiodarone should be avoided when possible.
Reference:
American Geriatrics Society 2015 Updated Beers Criteria for Potentially Inappropriate Medication Use in Older Adults. Journal of the American Geriatrics Society. 2015;63(11):2227-2246. doi:10.1111/jgs.13702.
Reference:
American Geriatrics Society 2015 Updated Beers Criteria for Potentially Inappropriate Medication Use in Older Adults. Journal of the American Geriatrics Society. 2015;63(11):2227-2246. doi:10.1111/jgs.13702.
Question 9 |
DR is a 81 year old female admitted in ICU with PNA, A Fib, CHF with preserved left ventricular function. She weighs 76 kg. She has history of lung cancer for which she is being treated with cyberknife and chemotherapy as outpatient, history of hypertension, hyperlipidemia, hypothyroidism, COPD. On admission her WBC is 1.0 K/uL, bands of 32% and segs of 42%. SR was started on Vancomycin, Levofloxacin and Aztreonam for HAP. She is also on the electrolyte replacement protocol. She is allergic to PCN/cephalosporin (rash). For her A. Fib she was given Amiodarone 400mg orally BID and Diltiazem 10mg/hr. She also received few doses of furosemide for her CHF.
What is DR’s ANC?
740 | |
500 | |
420 | |
320 |
Question 9 Explanation:
ANC = WBC * ((Segs/100) + (Bands/100)) ANC = 1.0 k/uL x (0.32 + 0.42) = 740
Reference:
Whalen KL, Borja-Hart N (2015). Interpretation of Clinical Laboratory Data. In: Nemire RE, Kier KL, Assa-Eley M. Nemire R.E., Kier K.L., Assa-Eley M Eds. Ruth E. Nemire, et al.eds. Pharmacy Student Survival Guide, 3e. New York, NY: McGraw-Hill; 2015.
Reference:
Whalen KL, Borja-Hart N (2015). Interpretation of Clinical Laboratory Data. In: Nemire RE, Kier KL, Assa-Eley M. Nemire R.E., Kier K.L., Assa-Eley M Eds. Ruth E. Nemire, et al.eds. Pharmacy Student Survival Guide, 3e. New York, NY: McGraw-Hill; 2015.
Question 10 |
DR is a 81 year old female admitted in ICU with PNA, A Fib, CHF with preserved left ventricular function. She weighs 76 kg. She has history of lung cancer for which she is being treated with cyberknife and chemotherapy as outpatient, history of hypertension, hyperlipidemia, hypothyroidism, COPD. On admission her WBC is 1.0 K/uL, bands of 32% and segs of 42%. SR was started on Vancomycin, Levofloxacin and Aztreonam for HAP. She is also on the electrolyte replacement protocol. She is allergic to PCN/cephalosporin (rash). For her A. Fib she was given Amiodarone 400mg orally BID and Diltiazem 10mg/hr. She also received few doses of furosemide for her CHF.
Physician would like to treat DR’s low ANC. Which of the following would be the treatment of choice with dose for her low ANC?
Filgrastim 380 mcg subcutaneously daily | |
Filgrastim 480 mcg subcutaneously daily | |
Erythropoietin 10,000 untis subcutaneously daily | |
Fresh Frozen Plasma (FFP) 15 mls/kg |
Question 10 Explanation:
Considering this patient had received chemotherapy (unable to determine when exactly), this dosage is consistent with the indication of primary prophylaxis in patients with nonmyeloid malignancies (5 mcg/kg/day subcutaneously).Erythropoietin is indicated for treatment of Anemia due to various causes. FFP is given in certain bleeding disorder to replace factors.
Reference:
Gold Standard, Inc. Filgrastim, G-CS. Clinical Pharmacology [database online]. Available at:https://www.clinicalpharmacology-ip.com/Forms/Monograph/monograph.aspx?cpnum=246&sec=monindi&t=0 Accessed: May 16, 2016.
Reference:
Gold Standard, Inc. Filgrastim, G-CS. Clinical Pharmacology [database online]. Available at:https://www.clinicalpharmacology-ip.com/Forms/Monograph/monograph.aspx?cpnum=246&sec=monindi&t=0 Accessed: May 16, 2016.
Question 11 |
DR is a 81 year old female admitted in ICU with PNA, A Fib, CHF with preserved left ventricular function. She weighs 76 kg. She has history of lung cancer for which she is being treated with cyberknife and chemotherapy as outpatient, history of hypertension, hyperlipidemia, hypothyroidism, COPD. On admission her WBC is 1.0 K/uL, bands of 32% and segs of 42%. SR was started on Vancomycin, Levofloxacin and Aztreonam for HAP. She is also on the electrolyte replacement protocol. She is allergic to PCN/cephalosporin (rash). For her A. Fib she was given Amiodarone 400mg orally BID and Diltiazem 10mg/hr. She also received few doses of furosemide for her CHF.
What significant drug / drug interaction do you identify?
Furosemide and Amiodarone | |
Vancomycin and Amiodarone | |
Aztreonam and Amiodarone | |
Levofloxacin and Amiodarone |
Question 11 Explanation:
There is a drug interaction between levofloxacin and amiodarone, which may increase the risk of QT prolongation. Levofloxacin is associated with QT prolongation and rarely torsades de pointes. Amiodarone also has a risk of QT prolongation and torsades de pointes. This drug interaction is possible for days to weeks after amiodarone is discontinued because amiodarone has a long half-life. There is also a drug interaction with furosemide and amiodarone. Caution must be used because loop diuretics can lower potassium and magnesium levels, which can cause amiodarone to not work effectively, but the patient is on electrolyte replacement protocol and on it for short duration.
Reference:
Gold Standard, Inc. Levofloxacin. Clinical Pharmacology [database online]. Available at:https://www.clinicalpharmacology-ip.com/Forms/Monograph/monograph.aspx?cpnum=746&sec=moninte&t=0. Accessed: May 18, 2016.
II. Gold Standard, Inc. Amiodarone. Clinical Pharmacology [database online]. Available at:https://www.clinicalpharmacology-ip.com/Forms/Monograph/monograph.aspx?cpnum=25&sec=moninte&t=0. Accessed: May 18, 2016.
Reference:
Gold Standard, Inc. Levofloxacin. Clinical Pharmacology [database online]. Available at:https://www.clinicalpharmacology-ip.com/Forms/Monograph/monograph.aspx?cpnum=746&sec=moninte&t=0. Accessed: May 18, 2016.
II. Gold Standard, Inc. Amiodarone. Clinical Pharmacology [database online]. Available at:https://www.clinicalpharmacology-ip.com/Forms/Monograph/monograph.aspx?cpnum=25&sec=moninte&t=0. Accessed: May 18, 2016.
Question 12 |
DR is a 81 year old female admitted in ICU with PNA, A Fib, CHF with preserved left ventricular function. She weighs 76 kg. She has history of lung cancer for which she is being treated with cyberknife and chemotherapy as outpatient, history of hypertension, hyperlipidemia, hypothyroidism, COPD. On admission her WBC is 1.0 K/uL, bands of 32% and segs of 42%. SR was started on Vancomycin, Levofloxacin and Aztreonam for HAP. She is also on the electrolyte replacement protocol. She is allergic to PCN/cephalosporin (rash). For her A. Fib she was given Amiodarone 400mg orally BID and Diltiazem 10mg/hr. She also received few doses of furosemide for her CHF.
DR’s TSH 0.041ulU/ml, she has been taking 125mcg of levothyroxine orally for more than a year. What would be the most appropriate drug regimen modification?
Increase dose of Levothyroxine to 150mcg oral daily | |
Decrease dose of levothyroxine to 100mcg oral daily | |
Increase dose of Levothyroxine to 150mcg IV daily | |
Decrease dose of levothyroxine to 100mcg IV daily |
Question 12 Explanation:
Decrease the dose to 100mcg orally daily. The TSH level is below therapeutic range (0.358--3.740 uIUn/mL). The TSH level is generally inversely related to the thyroid hormones’ levels. Bioequivalent of oral to intravenous levothyroxine is 2:1 ratio, so changing any dose to IV above 75mcg dose wound be to increase the dose.
Reference:
Bahn R, et al. hyperthyroidism and other causes of thyrotoxicosis: management guidelines of the american thyroid association and american association of clinical endocrinologists. EndocrPract. 2011;17(3). Available at: https://www.aace.com/files/hyper-guidelines-2011.pdf. Accessed May 18, 2016.
Reference:
Bahn R, et al. hyperthyroidism and other causes of thyrotoxicosis: management guidelines of the american thyroid association and american association of clinical endocrinologists. EndocrPract. 2011;17(3). Available at: https://www.aace.com/files/hyper-guidelines-2011.pdf. Accessed May 18, 2016.
Question 13 |
DR is a 81 year old female admitted in ICU with PNA, A Fib, CHF with preserved left ventricular function. She weighs 76 kg. She has history of lung cancer for which she is being treated with cyberknife and chemotherapy as outpatient, history of hypertension, hyperlipidemia, hypothyroidism, COPD. On admission her WBC is 1.0 K/uL, bands of 32% and segs of 42%. SR was started on Vancomycin, Levofloxacin and Aztreonam for HAP. She is also on the electrolyte replacement protocol. She is allergic to PCN/cephalosporin (rash). For her A. Fib she was given Amiodarone 400mg orally BID and Diltiazem 10mg/hr. She also received few doses of furosemide for her CHF.
Which of the following cardiovascular changes is/are seen as body ages?
Increase in total peripheral resistance | |
Increase in cardiac output | |
Increase in baroreceptor sensitivity | |
Increase in Beta-adrenergic receptor sensitivity |
Question 13 Explanation:
With aging, blood pressure and total peripheral resistance increase, however, a decrease in cardiac output is seen. A progressive decline in baroreceptor sensitivity is a characteristic feature of human aging as is a decrease in Beta-adrenergic receptor sensitivity.
Reference:
I. Martin WH 3rd e. Effects of aging, gender, and physical training on peripheral vascular function. - PubMed - NCBI. Ncbinlmnihgov. 2016. Available at: https://www.ncbi.nlm.nih.gov/pubmed/1860209. Accessed October 12, 2016.
II. O'Mahony D e. Reduced baroreflex sensitivity in elderly humans is not due to efferent autonomic dysfunction. - PubMed - NCBI. Ncbinlmnihgov. 2016. Available at: https://www.ncbi.nlm.nih.gov/pubmed/10600664. Accessed October 12, 2016.
III. Ferrara N, Komici K, Corbi G et al. β-adrenergic receptor responsiveness in aging heart and clinical implications. Frontiers in Physiology. 2014;4. doi:10.3389/fphys.2013.00396.
Reference:
I. Martin WH 3rd e. Effects of aging, gender, and physical training on peripheral vascular function. - PubMed - NCBI. Ncbinlmnihgov. 2016. Available at: https://www.ncbi.nlm.nih.gov/pubmed/1860209. Accessed October 12, 2016.
II. O'Mahony D e. Reduced baroreflex sensitivity in elderly humans is not due to efferent autonomic dysfunction. - PubMed - NCBI. Ncbinlmnihgov. 2016. Available at: https://www.ncbi.nlm.nih.gov/pubmed/10600664. Accessed October 12, 2016.
III. Ferrara N, Komici K, Corbi G et al. β-adrenergic receptor responsiveness in aging heart and clinical implications. Frontiers in Physiology. 2014;4. doi:10.3389/fphys.2013.00396.
Question 14 |
KL is a 76 year old female, who comes to the ER from a nursing home with SOB. Past medical history of COPD, DM, Schizophrenia, HTN. Chest x-ray upon admission showed pneumonic infiltrate in the left lower lung and possible early pneumonia in the right lung base. WBC 15.3 K/uL. Temp 102 F, HR 103 beats per minute, BP 134/65 mmHg, RR 40 breaths per minute. She was not on any antibiotics prior to admission. Her nursing home meds include Albuterol/Atrovent nebs, Amlodipine, Metformin, Risperidone, Glimepiride, Losartan and Prednisone.
What would be the appropriate antibiotics to treat her pneumonia?
Levofloxacin and Ceftriaxone | |
Levofloxacin and Piperacillin/Tazobactam | |
Piperacillin/Tazobactam, Cefepime, Vancomycin | |
Piperacillin/Tazobactam, and Vancomycin. |
Question 14 Explanation:
A and B are incorrect because there is no MRSA coverage, and this patient has risk of MDR because she came from a nursing home. C is incorrect because Piperacillin/Tazobactam and cefepime provide duplicate coverage for pseudomonas. D. is the correct answer because she came from a nursing home she should be treated as having healthcare-care associated pneumonia risk for MDR. She should be started on IV empiric therapy with Levofloxacin, Vancomycin, and Piperacillin/Tazobactam.
Reference:
Guidelines for the Management of Adults with Hospital-acquired, Ventilator-associated, and Healthcare-associated Pneumonia. Am J RespirCrit Care Med. 2005;171(4):388-416. doi:10.1164/rccm.200405-644st
Reference:
Guidelines for the Management of Adults with Hospital-acquired, Ventilator-associated, and Healthcare-associated Pneumonia. Am J RespirCrit Care Med. 2005;171(4):388-416. doi:10.1164/rccm.200405-644st
Question 15 |
KL is a 76 year old female, who comes to the ER from a nursing home with SOB. Past medical history of COPD, DM, Schizophrenia, HTN. Chest x-ray upon admission showed pneumonic infiltrate in the left lower lung and possible early pneumonia in the right lung base. WBC 15.3 K/uL. Temp 102 F, HR 103 beats per minute, BP 134/65 mmHg, RR 40 breaths per minute. She was not on any antibiotics prior to admission. Her nursing home meds include Albuterol/Atrovent nebs, Amlodipine, Metformin, Risperidone, Glimepiride, Losartan and Prednisone.
If it was a community acquired pneumonia transferred to ICU what would be the antibiotics of choice considering the patient has no penicillin allergy and no pseudomonas infections?
Azithromycin and Ceftriaxone | |
Levofloxacin and Vancomycin | |
Azithromycin, Vancomycin | |
Levofloxacin, Piperacillin/Tazobactam, and Vancomycin. |
Question 15 Explanation:
Answer A. is the correct answer because according to the IDSA CAP guidelines, antibiotics that should be started are a beta-lactam and either azithromycin or a fluoroquinolone for patients without penicillin allergy. For pseudomonas infections, empiric therapy can be with Piperacillin/Tazobactam plus levofloxacin or ciprofloxacin. B is wrong because this option does not include a beta-lactam. C and D are wrong because Piperacillin/Tazobactam is for pseudomonas infections. Vancomycin is inappropriate because this is community-acquired pneumonia and therefore the patient is not at risk for MRSA as he would be if he had healthcare or hospital acquired pneumonia.
Reference:
Mandell L, Wunderink R, Anzueto A et al. Infectious Diseases Society of America/American Thoracic Society Consensus Guidelines on the Management of Community-Acquired Pneumonia in Adults. Clinical Infectious Diseases. 2007;44(Supplement 2):S27-S72. doi:10.1086/511159.
Reference:
Mandell L, Wunderink R, Anzueto A et al. Infectious Diseases Society of America/American Thoracic Society Consensus Guidelines on the Management of Community-Acquired Pneumonia in Adults. Clinical Infectious Diseases. 2007;44(Supplement 2):S27-S72. doi:10.1086/511159.
Question 16 |
KL is a76 year old female, comes in the ER from nursing home with SOB. Past medical history of COPD DM, Schizophrenia, HTN. Chest x-ray upon admission showed pneumonic infiltrate in the left lower lung and possible early pneumonia in the right lung base. WBC 15.3 K/uL. Temp 102 F, HR 103 beats per minute, BP 134/65 mmHg, RR 40 breaths per minute. She was not on any antibiotics prior to admission. Her nursing home meds include, Albuterol/Atrovent nebs, Amlodipine, Metformin, Risperidone, Glimepiride, Losartan and Prednisone.
If it was a community acquired pneumonia and the patient was transferred to regular floor what would be the antibiotics of choice?
Levofloxacin and Azithromycin | |
Azithromycin alone | |
Levofloxacin and Ceftriaxone | |
Levofloxacin alone. |
Question 16 Explanation:
Antibiotic treatment can be with a respiratory fluoroquinolone (levofloxacin or ciprofloxacin) alone. Another option is to give ceftriaxone plus a macrolide such as Azithromycin. A and C are incorrect because Levofloxacin monotherapy is sufficient. B is incorrect because a macrolide should be given with a 3rd generation cephalosporin. Azithromycin and Levofloxacin provides overlap in atypical coverage.
Reference:
Guidelines for the Management of Adults with Hospital-acquired, Ventilator-associated, and Healthcare-associated Pneumonia. Am J RespirCrit Care Med. 2005;171(4):388-416. doi:10.1164/rccm.200405-644st.
Reference:
Guidelines for the Management of Adults with Hospital-acquired, Ventilator-associated, and Healthcare-associated Pneumonia. Am J RespirCrit Care Med. 2005;171(4):388-416. doi:10.1164/rccm.200405-644st.
Question 17 |
What is/are risk factors for Pseudomonal Pneumonia?
On mechanical ventilator for >5 days | |
10 years history COPD | |
Chronic steroid use | |
All of the Above |
Question 17 Explanation:
The IDSA guidelines for CAP PNA list risk factors specific for pseudomonas which are alcoholism, structural lung diseases, such as bronchiectasis, or repeated exacerbations of severe COPD leading to frequent steroid and/or antibiotic use, on mechanical ventilator for >3 days, as well as prior antibiotic therapy.
Reference:
Mandell L, Wunderink R, Anzueto A et al. Infectious Diseases Society of America/American Thoracic Society Consensus Guidelines on the Management of Community-Acquired Pneumonia in Adults. Clinical Infectious Diseases. 2007;44(Supplement 2):S27-S72. doi:10.1086/511159.
II. Guidelines for the Management of Adults with Hospital-acquired, Ventilator-associated, and Healthcare-associated Pneumonia. Am J RespirCrit Care Med. 2005;171(4):388-416. doi:10.1164/rccm.200405-644st.
Reference:
Mandell L, Wunderink R, Anzueto A et al. Infectious Diseases Society of America/American Thoracic Society Consensus Guidelines on the Management of Community-Acquired Pneumonia in Adults. Clinical Infectious Diseases. 2007;44(Supplement 2):S27-S72. doi:10.1086/511159.
II. Guidelines for the Management of Adults with Hospital-acquired, Ventilator-associated, and Healthcare-associated Pneumonia. Am J RespirCrit Care Med. 2005;171(4):388-416. doi:10.1164/rccm.200405-644st.
Question 18 |
What is/are the risk factor for MRSA pneumonia?
Prior exposure to Ciprofloxacin and Levofloxacin | |
Recent influenza infection | |
ESRD | |
All of Above |
Question 18 Explanation:
The ISDA guidelines for CAP PNA list risk factors specific for MRSA, which are end-stage renal disease, injection drug abuse, prior influenza, and prior antibiotic therapy, especially
with fluoroquinolones. Infection with the influenza virus has been shown to be a risk factor for MRSA. Other risk factors for multi-drug resistant HAP, VAP, and HCAP are previous use of antibiotics within the last 90 days, current hospitalization of 5 days or more, local high occurrence antibiotic resistance, immunosuppressive state, or risk factors for HCAP (2 or more days of hospitalization in past 30 days, residence in a long term care facility or nursing home, family member with multidrug-resistant pathogen, home wound care, family member with multidrug-resistant pathogen, chronic dialysis within the last 30 days, or home infusion therapy). Investigations have shown that fluoroquinolones are associated with predisposing patients to MRSA infections. Several case control studies demonstrate that exposure to either levofloxacin or ciprofloxacin use was associated with MRSA infection but not MSSA.
Reference:
I. Weber SG, Gold HS, Hooper DC, Karchmer AW, Carmeli Y. Fluoroquinolones and the Risk for Methicillin-resistant Staphylococcus aureus in Hospitalized Patients. Emerging Infectious Diseases. 2003;9(11):1415-1422. doi:10.3201/eid0911.030284
II. Mandell L, Wunderink R, Anzueto A et al. Infectious Diseases Society of America/American Thoracic Society Consensus Guidelines on the Management of Community-Acquired Pneumonia in Adults. Clinical Infectious Diseases. 2007;44(Supplement 2):S27-S72. doi:10.1086/511159.
Reference:
I. Weber SG, Gold HS, Hooper DC, Karchmer AW, Carmeli Y. Fluoroquinolones and the Risk for Methicillin-resistant Staphylococcus aureus in Hospitalized Patients. Emerging Infectious Diseases. 2003;9(11):1415-1422. doi:10.3201/eid0911.030284
II. Mandell L, Wunderink R, Anzueto A et al. Infectious Diseases Society of America/American Thoracic Society Consensus Guidelines on the Management of Community-Acquired Pneumonia in Adults. Clinical Infectious Diseases. 2007;44(Supplement 2):S27-S72. doi:10.1086/511159.
Question 19 |
Which of the following statements is true regarding calculating creatinine clearance in patients >65 years of age?
When serum creatinine value is less than 1mg/dl, serum creatinine should be rounded to 1 mg/dl. | |
Adjusted body weight should be used in morbidly obese patients to calculate creatinine clearance. | |
Actual serum creatinine should be used to calculate creatinine clearance | |
B and C. |
Question 19 Explanation:
An unbiased Cockcroft-Gault creatinine clearance can be calculated using actual body weight in underweight patients and ideal body weight in patients of normal weight. Using ABW(0.4) for overweight, obese, and morbidly obese patients appears to be the least biased and most accurate method for calculating their Cockcroft-Gault creatinine clearance. In addition, the common practice of rounding or replacing low Serum Creatinine values with an arbitrary value of 1.0 mg/dl for use in the CG equation should be avoided. Rounding S(c) (r) in patients with low S(c) (r) did not improve accuracy or bias of the creatinine clearance calculations.
Reference:
I. Dowling T, Wang E, Ferrucci L, Sorkin J. Glomerular Filtration Rate Equations Overestimate Creatinine Clearance in Older Individuals Enrolled in the Baltimore Longitudinal Study on Aging: Impact on Renal Drug Dosing. Pharmacotherapy: The Journal of Human Pharmacology and Drug Therapy. 2013;33(9):912-921. doi:10.1002/phar.1282.
II. Winter MA e. Impact of various body weights and serum creatinine concentrations on the bias and accuracy of the Cockcroft-Gault equation. - PubMed - NCBI. Ncbinlmnihgov. 2016. Available at: https://www.ncbi.nlm.nih.gov/pubmed/22576791. Accessed October 13, 2016.
Reference:
I. Dowling T, Wang E, Ferrucci L, Sorkin J. Glomerular Filtration Rate Equations Overestimate Creatinine Clearance in Older Individuals Enrolled in the Baltimore Longitudinal Study on Aging: Impact on Renal Drug Dosing. Pharmacotherapy: The Journal of Human Pharmacology and Drug Therapy. 2013;33(9):912-921. doi:10.1002/phar.1282.
II. Winter MA e. Impact of various body weights and serum creatinine concentrations on the bias and accuracy of the Cockcroft-Gault equation. - PubMed - NCBI. Ncbinlmnihgov. 2016. Available at: https://www.ncbi.nlm.nih.gov/pubmed/22576791. Accessed October 13, 2016.
Question 20 |
JP is a 66yr old male who was found lying on the floor with several empty liquor bottles by his friend. After being brought to the ER his serum alcohol level was found to be 475 mg/dl. Toxicology report is negative except for high alcohol levels. Two hours. after admission in the ER he was intubated and then transferred to the ICU . His liver enzymes and renal function is normal. PT/INR within normal limit. No past medical history. Upon transfer medications includes Propofol, MVI daily, Lorazepam prn and Piperacillin/Tazobactam.
What measures can be taken to prevent ventilator associated Pneumonia (VAP)?
Twice daily oral decontamination with Chlorhexidine | |
Give Pipercillin/Tazobactam 3.375gm IV q6hr prophylaxis | |
Elevate the head of the bed by 30-45 degrees. | |
A and C are appropriate measures to prevent VAP |
Question 20 Explanation:
The following 5 elements are part of the Institute of Healthcare Improvement VAP bundle: oral care with Chlorhexidine, head of bed elevation, DVT prophylaxis, SUP, and daily sedation assessment and spontaneous breathing trials. Other suggested measures for VAP prophylaxis are small bowel feeding instead of gastric feeding, prophylactic probiotics, alcohol based hand washing policy, early discontinuation of invasive devices, early tracheostomy, and reducing reintubation rates. Giving prophylaxis antibiotic is not recommended.
Reference:
Kalanuria AA, Zai W, Mirski M. Ventilator-associated pneumonia in the ICU. Critical Care. 2014;18(2):208. doi:10.1186/cc13775.
Reference:
Kalanuria AA, Zai W, Mirski M. Ventilator-associated pneumonia in the ICU. Critical Care. 2014;18(2):208. doi:10.1186/cc13775.
Question 21 |
JP is a 66yr old male who was found lying on the floor with several empty liquor bottles by his friend. After being brought to the ER his serum alcohol level was found to be 475 mg/dl. Toxicology report negative except for high alcohol level. 2 hrs. after admission in the ER he was intubated and then transferred to ICU . His liver enzymes and renal function is normal. PT/INR within normal limit. No past medical history. Upon transfer medications includes Propofol, MVI daily, Lorazepam prn and Piperacillin/Tazobactam.
What vitamin should the patient receive to avoid Wernicke- Korsakoff syndrome?
Thiamine | |
Cyanocobalamin | |
Magnesium | |
Folic Acid |
Question 21 Explanation:
Thiamine should be administered to prevent Wernicke’s encephalopathy.
Reference:
I. Management of moderate and severe alcohol withdrawal syndromes. Uptodate.com. 2016. Available at: http://www.uptodate.com/contents/management-of-moderate-and-severe-alcohol-withdrawal Accessed May 24, 2016.
Reference:
I. Management of moderate and severe alcohol withdrawal syndromes. Uptodate.com. 2016. Available at: http://www.uptodate.com/contents/management-of-moderate-and-severe-alcohol-withdrawal Accessed May 24, 2016.
Question 22 |
JP is a 66yr old male who was found lying on the floor with several empty liquor bottles by his friend. After being brought to the ER his serum alcohol level was found to be 475 mg/dl. Toxicology report negative except for high alcohol level. 2 hrs. after admission in the ER he was intubated and then transferred to ICU . His liver enzymes and renal function is normal. PT/INR within normal limit. No past medical history. Upon transfer medications includes Propofol, MVI daily, Lorazepam prn and Piperacillin/Tazobactam.
What is the treatment of choice for his acute alcohol withdrawal?
Haloperidol | |
Ativan | |
Ziprasidone | |
Alprazolam |
Question 22 Explanation:
Benzodiazepines are the most studied drugs for alcohol withdrawal treatment. Long-acting agents such as Diazepam and Chlordiazepoxide may be used. Antipsychotics are not recommended to treat alcohol withdrawal. Haloperidol and is an inappropriate choice.
Reference:
I. Kosten T, O’Connor P. Management of drug and alcohol withdrawal. N Engl J Med 2003;348:1786- 95. A good general review of the management of the most common syndromes.
II. Management of moderate and severe alcohol withdrawal syndromes. Uptodatecom. 2016. Available at: http://www.uptodate.com/contents/management-of-moderate-and-severe-alcohol-withdrawal-syndromes. Accessed May 24, 2016
Reference:
I. Kosten T, O’Connor P. Management of drug and alcohol withdrawal. N Engl J Med 2003;348:1786- 95. A good general review of the management of the most common syndromes.
II. Management of moderate and severe alcohol withdrawal syndromes. Uptodatecom. 2016. Available at: http://www.uptodate.com/contents/management-of-moderate-and-severe-alcohol-withdrawal-syndromes. Accessed May 24, 2016
Question 23 |
JP is a 66yr old male who was found lying on the floor with several empty liquor bottles by his friend. After being brought to the ER his serum alcohol level was found to be 475 mg/dl. Toxicology report negative except for high alcohol level. 2 hrs. after admission in the ER he was intubated and then transferred to ICU . His liver enzymes and renal function is normal. PT/INR within normal limit. No past medical history. Upon transfer medications includes Propofol, MVI daily, Lorazepam prn and Piperacillin/Tazobactam.
Which of the following would be appropriate chronic treatment of choice for his alcohol withdrawal?
Acamprosate | |
Metronidazole | |
Diazepam | |
Duloxetine |
Question 23 Explanation:
Acamprosate is indicated for ethanol dependence, but only in patients who have become abstinent. Diazepam is not indicated for ethanol dependence but for acute alcohol withdrawal. Metronidazole may interfere with the metabolism of ethanol, resulting in disulfiram-like effects. Patients should try to avoid ethanol ingestion to avoid the risk of undesirable side effects. Duloxetine is not indicated to treat alcohol withdrawal.
Reference:
I. Doering P, Boothby L. Substance-related disorders: overview and depressants, stimulants, and hallucinogens. In: DiPiro J, Talbert R, Yee G, et al., eds. Pharmacotherapy. A Pathophysiologic Approach, 7th ed. New York: McGraw-Hill, 2008.
II. Gold Standard, Inc. Acamprosate (Indications/Dosage). https://www.clinicalpharmacology-ip.com/Forms/Monograph/monograph.aspx?cpnum=2097&sec=monindi&t=0. Accessed May 24, 2016.
Reference:
I. Doering P, Boothby L. Substance-related disorders: overview and depressants, stimulants, and hallucinogens. In: DiPiro J, Talbert R, Yee G, et al., eds. Pharmacotherapy. A Pathophysiologic Approach, 7th ed. New York: McGraw-Hill, 2008.
II. Gold Standard, Inc. Acamprosate (Indications/Dosage). https://www.clinicalpharmacology-ip.com/Forms/Monograph/monograph.aspx?cpnum=2097&sec=monindi&t=0. Accessed May 24, 2016.
Question 24 |
JP is a 66yr old male who was found lying on the floor with several empty liquor bottles by his friend. After being brought to the ER his serum alcohol level was found to be 475 mg/dl. Toxicology report negative except for high alcohol level. 2 hrs. after admission in the ER he was intubated and then transferred to ICU . His liver enzymes and renal function is normal. PT/INR within normal limit. No past medical history. Upon transfer medications includes Propofol, MVI daily, Lorazepam prn and Piperacillin/Tazobactam.
Which of the following is/are major risk factors for VTE?
Surgery | |
Cancer | |
A and B | |
Alcohol consumption |
Question 24 Explanation:
Surgery, trauma (major trauma or lower-extremity injury), immobility, lower-extremity paresis, cancer (active or occult), cancer therapy (hormonal, chemotherapy, angiogenesis inhibitors, radiotherapy), venous compression (tumor, hematoma, arterial abnormality), previous VTE, increasing age, pregnancy and the postpartum period, estrogen-containing oral contraceptives or hormone replacement therapy, selective estrogen receptor modulators, erythropoiesis-stimulating agents, acute medical illness, inflammatory bowel disease, nephrotic syndrome, myeloproliferative disorders, paroxysmal nocturnal hemoglobinuria, obesity, central venous catheterization, and inherited or acquired thrombophilia.
Reference:
Prevention of Venous Thromboembolism*: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest. 2008;133(6_suppl):381S.
Reference:
Prevention of Venous Thromboembolism*: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest. 2008;133(6_suppl):381S.
Question 25 |
JP is a 66yr old male who was found lying on the floor with several empty liquor bottles by his friend. After being brought to the ER his serum alcohol level was found to be 475 mg/dl. Toxicology report negative except for high alcohol level. 2 hrs. after admission in the ER he was intubated and then transferred to ICU . His liver enzymes and renal function is normal. PT/INR within normal limit. No past medical history. Upon transfer medications includes Propofol, MVI daily, Lorazepam prn and Piperacillin/Tazobactam.
What is/are the indications for Stress Ulcer Prophylaxis (SUP)?
Patients with coagulopathy not related to anticoagulation use | |
Requirement for mechanical ventilator for over 48hrs | |
Use of high-dose corticosteroids (>250 mg of hydrocortisone or the equivalent per day | |
All of the above |
Question 25 Explanation:
SUP is indicated for patients who have coagulopathy, a requirement for mechanical ventilation for over 48 hours, a history of GI ulceration or bleeding within one year before admission, and in patients with at least two of the following: ICU stay of more than one week, sepsis, use of high-dose corticosteroids (>250 mg of hydrocortisone or the equivalent per day) and occult bleeding lasting six days or more.
Reference:
ASHP Therapeutic Guidelines on Stress Ulcer Prophylaxis. ASHP Commission on Therapeutics and approved by the ASHP Board of Directors on November 14, 1998. Am J Health Syst Pharm. 1999;56(4):347-379.
Reference:
ASHP Therapeutic Guidelines on Stress Ulcer Prophylaxis. ASHP Commission on Therapeutics and approved by the ASHP Board of Directors on November 14, 1998. Am J Health Syst Pharm. 1999;56(4):347-379.
Question 26 |
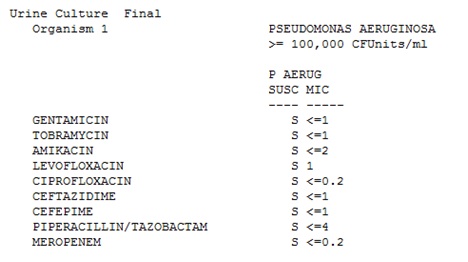
Patient comes in for sepsis syndrome secondary to aspiration pneumonia. He is given empiric therapy with levofloxacin, piperacillin/tazobactam and vancomycin. Sputum Culture grew the following:
Culture, Sputum Final
Organism 1 BETA STREPTOCOCCUS GROUP G
Moderate
Uniformly susceptible to Ampicillin and Penicillin
Organism 2 PROTEUS MIRABILIS
Few
GENTAMICIN S <=1
AMPICILLIN S <=2
TRIMETH/SULFA S <=20
CEFTRIAXONE S <=1
TOBRAMYCIN S <=1
AMIKACIN S <=2
LEVOFLOXACIN R >=8
CIPROFLOXACIN R >=4
AMP/SULBACTAM S <=2
CEFTAZIDIME S <=1
CEFEPIME S <=1
PIPERACILLIN/TAZOBAC S <=4
MEROPENEM S <=0.2
What is the best antimicrobial targeted therapy for this patient?
Continue the levofloxacin and piperacillin/Tazobactam, d/c other antibiotics | |
Continue the piperacillin/Tazobactam only, d/c other antibiotics | |
Initiate Ampicillin only, d/c other antibiotics | |
Initiate Meropenem, d/c other antibiotics |
Question 26 Explanation:
Piperacillin/Tazobactam and Meropenem are broad spectrum antibiotics. Levofloxacin should not be continued because the P. Mirabilis is resistant to it. Ampicillin is appropriate because both the P. Mirabilis and strep group G strain are susceptible to Ampicillin, and it has the narrowest spectrum of activity.
Reference:
Gilbert D. The Sanford Guide to Antimicrobial Therapy 2014. Sperryville, Va.: Antimicrobial Therapy; 2014.
Reference:
Gilbert D. The Sanford Guide to Antimicrobial Therapy 2014. Sperryville, Va.: Antimicrobial Therapy; 2014.
Question 27 |
The elimination half-life of which lipophilic drug is significantly prolonged due to an increase in volume of distribution in elderly patients?
Alprazolam
| |
Diazepam
| |
Lorazepam
| |
Triazolam
|
Question 27 Explanation:
The main effect of an increased volume of distribution is a prolongation of half-life. An increase VD and half-life have been observed for agents such as diazepam. Although, in general, the volume of distribution of most benzodiazepines tends to increase with age, for reason that are not clear, the VD of alprazolam (short half-life BZD) specifically decreases in elderly men but remains unchanged in elderly women. Triazolam is also considered to have a short half-life, compared to diazepam (highly lipophilic). Phase 2 reactions usually involve conjugation of phase 1 metabolites and appear to be unchanged by the ageing process although they may be impaired in some frail elderly people, an example of this would be lorazepam (no accumulation due to inactive metabolites.)
Reference:
I. Mangoni AJackson S. Age-related changes in pharmacokinetics and pharmacodynamics: basic principles and practical applications. British Journal of Clinical Pharmacology. 2003;57(1):6-14. doi:10.1046/j.1365-2125.2003.02007.x.
II. Summary of the Updated American Geriatrics Society/British Geriatrics Society clinical practice guideline for prevention of falls in older persons. J Am Geriatr Soc 2011;59:148-57.
Reference:
I. Mangoni AJackson S. Age-related changes in pharmacokinetics and pharmacodynamics: basic principles and practical applications. British Journal of Clinical Pharmacology. 2003;57(1):6-14. doi:10.1046/j.1365-2125.2003.02007.x.
II. Summary of the Updated American Geriatrics Society/British Geriatrics Society clinical practice guideline for prevention of falls in older persons. J Am Geriatr Soc 2011;59:148-57.
Question 28 |
Which of the following statements is true regarding piperacillin-tazobactam and ampicillin-sulbactam?
Piperacillin-tazobactam covers Acinetobacter, ampicillin-sulbactam does not. | |
Piperacillin-tazobactam covers ESBL, ampicillin-sulbactam does not. | |
Piperacillin-tazobactam covers pseudomonas, Ampicillin-sulbactam covers Acinetobacter. | |
Neither Piperacillin-tazobactam or ampicillin-sulbactam has anaerobic coverage |
Question 28 Explanation:
A is wrong because ampicillin-sulbactam covers Acinetobacter and piperacillin-tazobactam has variable coverage for Acinetobacter. B. is wrong because neither ampicillin-sulbactam nor piperacillin-tazobactam covers ESBL. D. is wrong because both ampicillin-sulbactam and piperacillin-tazobactam cover anaerobes.
Reference:
Gilbert D. The Sanford Guide to Antimicrobial Therapy 2014. Sperryville, Va.: Antimicrobial Therapy; 2014.
Reference:
Gilbert D. The Sanford Guide to Antimicrobial Therapy 2014. Sperryville, Va.: Antimicrobial Therapy; 2014.
Question 29 |
A patient comes in with urosepsis with risk factors for ESBL. What is the best empiric therapy?
Meropenem | |
Piperacillin-Tazobactam | |
Ceftriaxone | |
Ampicillin-Sulbactam |
Question 29 Explanation:
Meropenem is the drug of choice for ESBL empirically due to higher percentage of sensitivity. It can be de-escalated once culture and sensitivity available.
Reference:
Gilbert D. The Sanford Guide to Antimicrobial Therapy 2014. Sperryville, Va.: Antimicrobial Therapy; 2014
Reference:
Gilbert D. The Sanford Guide to Antimicrobial Therapy 2014. Sperryville, Va.: Antimicrobial Therapy; 2014
Question 30 |
Which of the following are risk factors for Clostridium difficile?
Advanced age | |
Previous antimicrobial usage | |
Use of acid-suppressing medications. | |
All of the Above |
Question 30 Explanation:
Advanced age, previous antimicrobial usage, duration of hospitalization, cancer chemotherapy, GI surgery, tube feeding, and use of acid-suppressing medications.
Reference:
Cohen S, Gerding D, Johnson S et al. Clinical Practice Guidelines for Clostridium difficile Infection in Adults: 2010 Update by the Society for Healthcare Epidemiology of America (SHEA) and the Infectious Diseases Society of America (IDSA). Infection Control and Hospital Epidemiology. 2010;31(5):431-455. Doi: 10.1086/651706
Reference:
Cohen S, Gerding D, Johnson S et al. Clinical Practice Guidelines for Clostridium difficile Infection in Adults: 2010 Update by the Society for Healthcare Epidemiology of America (SHEA) and the Infectious Diseases Society of America (IDSA). Infection Control and Hospital Epidemiology. 2010;31(5):431-455. Doi: 10.1086/651706
Question 31 |
In a study where rivaroxaban was compared to enoxaparin to find total VTE following hip replacement surgery, there were 17 total VTE out of 1513 patients in the rivaroxaban group and 57 total VTE out of 1473 patient in the enoxaparin group. What is the absolute risk reduction of using Rivaroxaban over Enoxaparin?
17 | |
57 | |
71 | |
2.7 |
Question 31 Explanation:
Absolute risk reduction: 0.027 = 2.7%
(Event rate in enoxaparin group) – (Event rate in rivaroxaban group) = (57/1473) – (17/1513) = 0.02746
Reference:
Barratt A, Wyer PC, Hatala R, et al. Tips for learners of evidence-based medicine: 1. Relative risk reduction, absolute risk reduction and number needed to treat. CMAJ. 2004;171(4):353-8. doi: 10.1503/cmaj.1021197.
(Event rate in enoxaparin group) – (Event rate in rivaroxaban group) = (57/1473) – (17/1513) = 0.02746
Reference:
Barratt A, Wyer PC, Hatala R, et al. Tips for learners of evidence-based medicine: 1. Relative risk reduction, absolute risk reduction and number needed to treat. CMAJ. 2004;171(4):353-8. doi: 10.1503/cmaj.1021197.
Question 32 |
Which of the following is a risk factor for myopathy with statin therapy?
Hypothyroidism | |
Vitamin D deficiency | |
Renal impairment | |
All of the above are risk factor |
Question 32 Explanation:
Risk factors for myopathy are hypothyroidism, reduced renal or hepatic function, and rheumatologic disorders such as polymyalgia rheumatica, steroid myopathy, vitamin D deficiency, or primary muscle diseases.
Reference:
Stone N, Robinson J, Lichtenstein A et al. 2013 ACC/AHA Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults. Circulation. 2013;129(25 suppl 2):S1-S45. doi:10.1161/01.cir.0000437738.63853.7a.
Reference:
Stone N, Robinson J, Lichtenstein A et al. 2013 ACC/AHA Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults. Circulation. 2013;129(25 suppl 2):S1-S45. doi:10.1161/01.cir.0000437738.63853.7a.
Question 33 |
Which of the following is considered first-line therapy for reducing the risk of atherosclerotic cardiovascular disease (ASCVD)?
HMG Co-A reductase inhibitors | |
Bile acid resins | |
Nicotinic Acid | |
Fibrates |
Question 33 Explanation:
ACC/AHA 2013 found that the use of statins for prevention of ASCVD is extensive and consistent. Statin therapy is recommended for patients at a higher risk of ASCVD who are most likely to experience a net benefit in terms of the potential for risk reduction vs the potential for adverse effects. Nonstatin therapies do not provide sufficient benefits in the reduction of ASCVD risk in regards to their potential for adverse effects.
Reference:
Stone N, Robinson J, Lichtenstein A et al. 2013 ACC/AHA Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults. Circulation. 2013;129(25 suppl 2):S1-S45. doi:10.1161/01.cir.0000437738.63853.7a.
Reference:
Stone N, Robinson J, Lichtenstein A et al. 2013 ACC/AHA Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults. Circulation. 2013;129(25 suppl 2):S1-S45. doi:10.1161/01.cir.0000437738.63853.7a.
Question 34 |
Which of the following clinical laboratory tests should be ordered and evaluated if a patient complains of unexplained severe muscle symptoms or fatigue while on statin therapy?
Total Bilirubin | |
Creatine Phosphokinase | |
Complete Blood Count | |
Liver function tests |
Question 34 Explanation:
Creatine Phosphokinase (CPK) should be evaluated if a patient experiences unexplained severe muscle symptoms or fatigue while receiving statin therapy.
Reference:
Stone N, Robinson J, Lichtenstein A et al. 2013 ACC/AHA Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults. Circulation. 2013;129(25 suppl 2):S1-S45. doi:10.1161/01.cir.0000437738.63853.7a.
Reference:
Stone N, Robinson J, Lichtenstein A et al. 2013 ACC/AHA Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults. Circulation. 2013;129(25 suppl 2):S1-S45. doi:10.1161/01.cir.0000437738.63853.7a.
Question 35 |
A Patient is receiving Piperacillin-Tazobactam for complicated UTI. Her allergies are sulfa and Moxifloxacin. What would be the most appropriate agent for de-escalation based on the C+S report?
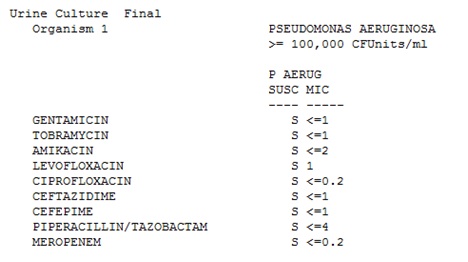
Cefepime | |
Continue piperacillin-tazobactam | |
Ciprofloxacin | |
Meropenem |
Question 35 Explanation:
Cefepime coverage is narrower than that of piperacillin-tazobactam and the culture is sensitive to Cefepime. Ciprofloxacin is not appropriate due to patient’s allergy to moxifloxacin.
Reference:
Gilbert D. The Sanford Guide to Antimicrobial Therapy 2014. Sperryville, Va.: Antimicrobial Therapy; 2014.
Reference:
Gilbert D. The Sanford Guide to Antimicrobial Therapy 2014. Sperryville, Va.: Antimicrobial Therapy; 2014.
Question 36 |
JP 77 YOWM with a history of hypertension, just got admitted for ischemic stroke. What would be the most appropriate pharmacotherapy recommendation upon discharge?
Atorvastatin 20 mg PO QHS | |
Pitavastatin 1 mg PO QHS | |
Atorvastatin 80 mg PO QHS | |
Lovastatin 20 mg PO QHS |
Question 36 Explanation:
A stroke falls under the category of clinical ASCVD, which includes acute coronary syndromes, or a history of MI, stable or unstable angina, coronary or other arterial revascularization, stroke, TIA, or peripheral arterial disease presumed to be of atherosclerotic origin. Patients with clinical ASCVD are at an increased risk for recurrent ASCVD and ASCVD death. This patient is under 75 years old, and such patients with clinical ASCVD should receive moderate-intensity statin therapy. Given the options above, a high intensity statin is the most appropriate option. The decision to start at the 80 mg dose of atorvastatin instead of the 40 mg dose is based on the recommendation to down titrate if the patient is unable to tolerate the 80 mg dose as opposed to up-titrating in accordance with the IDEAL trial.
Reference:
Stone N, Robinson J, Lichtenstein A et al. 2013 ACC/AHA Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults. Circulation. 2013;129(25 suppl 2):S1-S45. doi:10.1161/01.cir.0000437738.63853.7a.
Reference:
Stone N, Robinson J, Lichtenstein A et al. 2013 ACC/AHA Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults. Circulation. 2013;129(25 suppl 2):S1-S45. doi:10.1161/01.cir.0000437738.63853.7a.
Question 37 |
TM is a 78 YOW with a history of hypertension, hypercholesterolemia and arthritis was admitted for proximal arterial fibrillation. While in the hospital she was placed on diltiazem drip and eventually, converted to oral diltiazem 240mg. Pt’s home medication includes simvastatin 40mg po daily , hydrochlorothiazide 25mg po daily , lisinopril 20mg daily and acetaminophen. Her LDL-C is 100mg /dL. What would be the most appropriate change to make on her therapy?
Increase simvastatin to 80mg po daily | |
Keep simvastatin at 40mg po daily | |
Change simvastatin 40mg to atorvastatin 40mg po daily | |
Change simvastatin to lovastatin 20mg po daily |
Question 37 Explanation:
Diltiazem has a major drug interaction with simvastatin. Diltiazem is a CYP3A4 inhibitor, and since simvastatin is metabolized by CYP3A4, its level can build up and the risk of myopathy increases. Clinical Pharmacology recommends the use of switching to a non-CYP3A inhibitor such as pitavastatin, pravastatin, or rosuvastatin, and if simvastatin is to be kept on it should not exceed 10 mg/day. The same interaction also exists with lovastatin, and the recommendation is to not exceed a total dose of
20 mg/day po of lovastatin. Given the current options, the best choice is to change to Atorvastatin 40 mg po daily.
Reference:
I. Gold Standard, Inc. Lovastatin (Interactions). Clinical Pharmacology [database online]. Available at: https://www.clinicalpharmacology-ip.com/Forms/Monograph/monograph.aspx?cpnum=359&sec=moninte&t=0. Accessed: June 1, 2016
II. Gold Standard, Inc. Simvastatin (Interactions). Clinical Pharmacology [database online]. Available at: https://www.clinicalpharmacology-ip.com/Forms/Monograph/monograph.aspx?cpnum=565&sec=moninte&t=0. Accessed: June 1, 2016
Reference:
I. Gold Standard, Inc. Lovastatin (Interactions). Clinical Pharmacology [database online]. Available at: https://www.clinicalpharmacology-ip.com/Forms/Monograph/monograph.aspx?cpnum=359&sec=moninte&t=0. Accessed: June 1, 2016
II. Gold Standard, Inc. Simvastatin (Interactions). Clinical Pharmacology [database online]. Available at: https://www.clinicalpharmacology-ip.com/Forms/Monograph/monograph.aspx?cpnum=565&sec=moninte&t=0. Accessed: June 1, 2016
Question 38 |
Which of the following medications may increase LDL?
Lisinopril | |
Hydrochlorothiazide | |
Diltiazem | |
Acetaminophen |
Question 38 Explanation:
LDL can be elevated by diuretics, cyclosporine, glucocorticoids, and amiodarone.
Reference:
Stone N, Robinson J, Lichtenstein A et al. 2013 ACC/AHA Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults. Circulation. 2013; 129(25 suppl 2):S1-S45. doi:10.1161/01.cir.0000437738.63853.7a.
Reference:
Stone N, Robinson J, Lichtenstein A et al. 2013 ACC/AHA Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults. Circulation. 2013; 129(25 suppl 2):S1-S45. doi:10.1161/01.cir.0000437738.63853.7a.
Question 39 |
In the ARISTOTLE study the rate of death from any cause was 3.52% in Apixaban group per year Vs 3.94% in warfarin group. HR 0.89; 95% CI, 0.80 to 0.99. Which of the following statement is true based on the given information?
The rate of death from any cause was lower in the Apixaban group than in Warfarin group. | |
The rate of death from any cause was not significant in the Apixaban group Vs Warfarin group. | |
Warfarin had significantly lower rate of death compared to Apixaban. | |
Since there is no p value no conclusion can be drawn from the given data |
Question 39 Explanation:
A Is correct because the rate of death is significant as indicated by the 95% CI does not contain the value 1. So it is appropriate to make a statement: The rate of death from any cause was lower in the Apixaban group than in Warfarin group the meaning of 1 in a confidence ration indicates that the risk reduction in the outcome is the same between the two groups. Answer C is wrong because the rate of death in the warfarin group was higher than the rate in the apixaban group (3.94% vs 3.52% perspectively). Answer D is wrong because although there is no p value listed, statistical significance can still be inferred from a 95% confidence interval, which is presented here as 0.80 to 0.99.
Reference:
Windish DM, Huot SJ, Green ML. Medicine resident’s understanding of the biostatistics and results in the medical literature. JAMA 2007;298:1010-22.
Reference:
Windish DM, Huot SJ, Green ML. Medicine resident’s understanding of the biostatistics and results in the medical literature. JAMA 2007;298:1010-22.
Question 40 |
In the ARISTOTLE study the rate of the primary outcome was 1.27% per year in the apixaban group, as compared with 1.60% per year in the warfarin group (hazard ratio with apixaban, 0.79; 95% confidence interval [CI], 0.66 to 0.95; P<0.001 for noninferiority. The primary objective was to determine whether apixaban was noninferior to warfarin in reducing the rate of stroke (ischemic or hemorrhagic) or systemic embolism among patients with atrial fibrillation and at least one other risk factor for stroke. Which of the following statements is true based on the given information?
Apixaban is superior to warfarin in reducing rate of stroke or systemic embolism among patients with atrial fibrillation. | |
Apixaban is as effective as warfarin in reducing rate of stroke or systemic embolism among patients with atrial fibrillation. | |
Apixaban is more effective than warfarin in reducing rate of stroke but not systemic embolism among patients with atrial fibrillation | |
Apixaban is superior to warfarin in reducing rate of stroke but warfarin is noninferior in reducing systemic embolism among patients with atrial fibrillation. |
Question 40 Explanation:
Answer A is incorrect because presented p-value is for noninferiority, not for superiority. Based on the given information, no conclusions about superiority can be made. Answer B. is correct. The p-value provided is for noninferiority, it can be concluded that Apixaban is as effective as warfarin in reducing rate of stroke or systemic embolism among patients with atrial fibrillation. Answer C is incorrect. Stroke and systemic embolism were combined into one primary outcome here for this confidence interval, so more information is needed to determine which agent did better for the specific type of event, either stroke or systemic embolism. Answer D. is incorrect because the rate of the primary outcome was higher in the warfarin group compared to the apixaban group, meaning stroke or systemic embolism occurred more so in the warfarin group. For the same reason as with C, these two events are represented as combined into one primary outcome and more information would be needed.
Reference: I. Windish DM, Huot SJ, Green ML. Medicine resident’s understanding of the biostatistics and results in the medical literature. JAMA 2007;298:1010-22.
Reference: I. Windish DM, Huot SJ, Green ML. Medicine resident’s understanding of the biostatistics and results in the medical literature. JAMA 2007;298:1010-22.
Question 41 |
In the ARISTOTLE study the rate of systemic embolism was 0.09% in Apixaban group per year Vs 0.10% in warfarin group. HR 0.87; 95% CI, 0.44 to 1.75. Which of the following statements is true based on the given information?
There was statistically significant difference between Apixaban and warfarin group in reducing systemic embolism. | |
There was no statistically significant difference between Apixaban and warfarin group in reducing systemic embolism. | |
Statistical significance cannot be determined since there is no p value. | |
There was clinically significant difference between Apixaban and warfarin group in reducing systemic embolism. |
Question 41 Explanation:
Answer A is false because there is a difference between the two groups, but it is not statistically significant due to the 95% confidence interval containing 1. Answer C is wrong because although there is no p value listed, statistical significance can still be inferred from a 95% confidence interval. Answer D incorrect because usually, statistical significance should be demonstrated before considering clinical significance. There is a difference in the rate of systemic embolism, but it is so small (0.01%) that other factors of the two agents would weigh more in a decision to use one over the other.
Reference: DiCenzo R, ed. Clinical Pharmacist’s Guide to Bio¬statistics and Literature Evaluation. Lenexa, KS: ACCP, 2010.
Answer A is false because there is a difference between the two groups, but it is not statistically significant due to the 95% confidence interval containing 1. Answer C is wrong because although there is no p value listed, statistical significance can still be inferred from a 95% confidence interval. Answer D incorrect because usually, statistical significance should be demonstrated before considering clinical significance. There is a difference in the rate of systemic embolism, but it is so small (0.01%) that other factors of the two agents would weigh more in a decision to use one over the other. Reference:
Windish DM, Huot SJ, Green ML. Medicine resident’s understanding of the biostatistics and results in the medical literature. JAMA 2007;298:1010-22.
Reference: DiCenzo R, ed. Clinical Pharmacist’s Guide to Bio¬statistics and Literature Evaluation. Lenexa, KS: ACCP, 2010.
Answer A is false because there is a difference between the two groups, but it is not statistically significant due to the 95% confidence interval containing 1. Answer C is wrong because although there is no p value listed, statistical significance can still be inferred from a 95% confidence interval. Answer D incorrect because usually, statistical significance should be demonstrated before considering clinical significance. There is a difference in the rate of systemic embolism, but it is so small (0.01%) that other factors of the two agents would weigh more in a decision to use one over the other. Reference:
Windish DM, Huot SJ, Green ML. Medicine resident’s understanding of the biostatistics and results in the medical literature. JAMA 2007;298:1010-22.
Question 42 |
JK is a 68 YOM who comes in the hospital with acute exacerbation of heart failure. 4 days later his heart failure is stabilized and he feels much better. His ejection fraction is 30-35%. JK is currently on lisinopril 5mg daily, carvedilol 6.5mg orally twice daily, furosemide 20mg orally daily. Vitals are with in normal limits. CMP and CBC are also with in normal limits. Adding what medication may provide a reduction in mortality and morbidity?
Digoxin | |
Valsartan | |
Spironolactone | |
Hydralazine |
Question 42 Explanation:
Adding spironolactone may provide reduction in mortality and morbidity. Since JK has an ejection fraction of 30-35%, spironolactone would be appropriate since it is recommended for patients with an LVEF of 35% or less to reduce morbidity and mortality.
Digoxin does not reduce mortality or morbidity. However, it can be beneficial in decreasing hospitalizations for HF. JK is already taking lisinopril. Therefore, Valsartan would not be added. Use of both an ACE inhibitor and an ARB may result in potentially harmful adverse effects such as hypotension, renal dysfunction, and hyperkalemia. The use of Hydralazine in combination with Isosorbide Dinitrate is recommended in African Americans with NYHA class III-IV HFrEF, who have received optimal therapy with ACE inhibitors and beta-blockers, to reduce morbidity and mortality. Hydralazine alone has no benefit in reducing morbidity and mortality.
Reference:
Yancy CW, Jessup M, Bozkurt B, et al. 2013 ACCF/AHA Guideline for the Management of Heart Failure: Executive Summary: A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am CollCardiol. 2013;62(16):1495-1539. doi:10.1016/j.jacc.2013.05.020.
Reference:
Yancy CW, Jessup M, Bozkurt B, et al. 2013 ACCF/AHA Guideline for the Management of Heart Failure: Executive Summary: A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am CollCardiol. 2013;62(16):1495-1539. doi:10.1016/j.jacc.2013.05.020.
Question 43 |
What are the contraindications for using aldosterone receptor antagonist in a patient with congestive heart failure?
Serum creatinine greater than 2.5mg/dl | |
Potassium greater than 5mEq/L | |
A and B | |
Aldosterone 2 ng/dl (normal 4-31 ng/dl) |
Question 43 Explanation:
The contraindications for using aldosterone receptor antagonists in a patient with congestive heart failure are a serum creatinine > 2.5 mg/dL and a potassium level > 5 mEq/L. A potassium level > 5 mEq/L may result in life-threatening hyperkalemia. A serum creatinine > 2.5 mg/dL in men may indicate worsening renal function, which may lead to discontinuation of the aldosterone receptor antagonist.
Aldosterone levels are not considered a contraindication for using aldosterone receptor antagonists in those patients with congestive heart failure.
Reference:
Yancy CW, Jessup M, Bozkurt B, et al. 2013 ACCF/AHA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines.J Am CollCardiol. 2013;62(16):e147-e239. doi:10.1016/j.jacc.2013.05.019.
Reference:
Yancy CW, Jessup M, Bozkurt B, et al. 2013 ACCF/AHA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines.J Am CollCardiol. 2013;62(16):e147-e239. doi:10.1016/j.jacc.2013.05.019.
Question 44 |
JM is a 70 YOM admitted to the hospital with dyspnea and bilateral pedal edema. Past medical history includes hypertension and dyslipidemia. His HR is 85, two average BP 152/95. RR 35. His medications includes atorvastatin 40mg orally at bedtime and lisinopril 20mg daily. Echocardiogram showed 35-40% of EF. After a few doses of bumetanide JM's fluid status was normal his dyspnea and pedal edema was gone. Which of the following medications would be most appropriate to give in addition to lisinopril and atorvastatin?
Add Metoprolol Succinate | |
Add Spironolactone | |
Add bumetanide | |
Add hydrochlorothiazide |
Question 44 Explanation:
Adding the beta-blocker, metoprolol succinate, would be most appropriate to give in addition to lisinopril and atorvastatin. Initiation of a beta-blocker in a hospitalized patient is recommended after optimization of fluid status and once IV diuretics have been discontinued. Since the patient is stable, adding metoprolol succinate would be appropriate. Use of a beta-blocker has also been proven to reduce morbidity and mortality.
Diuretics would be prescribed to patients who have evidence of fluid retention, to treat relieve symptoms. Therefore, spironolactone, bumetanide, and hydrochlorothiazide would not be given since the patient is now stable. Fluid status is normal and his edema has resolved.
Reference:
Yancy CW, Jessup M, Bozkurt B, et al. 2013 ACCF/AHA Guideline for the Management of Heart Failure: Executive Summary: A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am CollCardiol. 2013;62(16):1495-1539. doi:10.1016/j.jacc.2013.05.020.
Diuretics would be prescribed to patients who have evidence of fluid retention, to treat relieve symptoms. Therefore, spironolactone, bumetanide, and hydrochlorothiazide would not be given since the patient is now stable. Fluid status is normal and his edema has resolved.
Reference:
Yancy CW, Jessup M, Bozkurt B, et al. 2013 ACCF/AHA Guideline for the Management of Heart Failure: Executive Summary: A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am CollCardiol. 2013;62(16):1495-1539. doi:10.1016/j.jacc.2013.05.020.
Question 45 |
JW is a 66 year old woman with a past medical history of gastroesophageal reflux disease, hypertension who got discharged from the hospital after a thrombotic stroke. JW is currently on lisinopril 20mg twice daily, pantoprazole 40mg daily and clopidogrel 75mg daily. Her fasting lipid profile is TC 201 mg/dL; LDL-C 102; HDL-C 48 mg/dL; and TG 62 mg/dL. Which is the best pharmacologic agent to initiate on JW?
Simvastatin 20mg daily | |
Atorvastatin 80mg daily | |
Atorvastatin 40mg daily | |
Atorvastatin 20mg daily |
Question 45 Explanation:
Because she just had a stroke, which is considered ASCVD, this patient is a candidate for statin therapy. Because she is less than 75 years old, she should receive a high intensity statin, which B and C fall under. 80 mg of atorvastatin has been shown to reduce LDL counts by more than 50%, and 40 mg was only tested in one RCT. It is better to start at the higher dose of 80 mg and down titrate if the patient experiences intolerance.
Reference:
Stone N, Robinson J, Lichtenstein A et al. 2013 ACC/AHA Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults. Circulation. 2013;129(25 suppl 2):S1-S45. doi:10.1161/01.cir.0000437738.63853.7a
Reference:
Stone N, Robinson J, Lichtenstein A et al. 2013 ACC/AHA Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults. Circulation. 2013;129(25 suppl 2):S1-S45. doi:10.1161/01.cir.0000437738.63853.7a
Question 46 |
JK is a 67 years African American man who presents to your clinic for his blood pressure management. His past medical history includes peptic ulcer disease and hypertension. His two BP readings are 160/98, 159/96 and HR 85. He says he has been adherent to his medication and lifestyle. He currently takes 12.5mg Chlorthalidone and Prilosec 20mg daily. Which of the following is the best strategy to manage his blood pressure?
Increase chlorthalidone to 25mg daily | |
Add Norvasc 2.5 daily | |
Add Lisinopril 5mg daily | |
Strategies A or B could be used |
Question 46 Explanation:
As the patient is over the age of 60 and he does not have CKD or diabetes, his goal BP should be SBP< 150 mmHg or DBP < 90 mmHg, and he is not currently at this goal with his medication regimen. Options are to maximize the current medication dosage (option A), or to add a second agent. Since calciumchannel blockers like Norvasc are recommended as initial treatment options in African Americans, choosing Norvasc over lisinopril would probably be the more effective option.
Reference:
James P, Oparil S, Carter B et al. 2014 Evidence-Based Guideline for the Management of High Blood Pressure in Adults. JAMA. 2014;311(5):507. doi:10.1001/jama.2013.284427.
Reference:
James P, Oparil S, Carter B et al. 2014 Evidence-Based Guideline for the Management of High Blood Pressure in Adults. JAMA. 2014;311(5):507. doi:10.1001/jama.2013.284427.
Question 47 |
A 69 years old African American male with a history of chronic kidney disease and osteoarthritis presents to your clinic. His two average BP readings are 146/87 mm Hg, HR is 65. His CBC and CMP are within normal limits. Which of the following is the best way to manage his hypertension?
Lifestyle modification | |
Lifestyle modification and lisinopril 2.5mg daily | |
Lifestyle modification and amlodipine 2.5mg daily | |
Life style modification and metoprolol succinate 25mg daily |
Question 47 Explanation:
The best option is B because this includes an ACE-inhibitor. His goal BP is SBP <140 mmHg and DBP < 90 mmHg, so he should be treated with pharmacological therapy since his SPB is above 140 mmHg. It is recommended that patients with CKD should receive an ACE-inhibitor or an ARB as initial or added-on therapy regardless of race.
Reference:
James P, Oparil S, Carter B et al. 2014 Evidence-Based Guideline for the Management of High Blood Pressure in Adults. JAMA. 2014;311(5):507. doi:10.1001/jama.2013.284427.
Reference:
James P, Oparil S, Carter B et al. 2014 Evidence-Based Guideline for the Management of High Blood Pressure in Adults. JAMA. 2014;311(5):507. doi:10.1001/jama.2013.284427.
Question 48 |
MK is a 67 YOM (No known drug allergy) admitted to ICU with VAP after staying in progressive care unit for 5 days for CHF, AECOPD and community acquired pneumonia. His vitals are within normal limits. According to your hospital antibiogram> 90 % of pseudomonas aeruginosa are sensitive to cefepime, piperacillin-tazobactam and meropenem and 70% of S. aureus isolates are methicillin resistance. What empiric antibiotic would be appropriate for MK?
piperacillin-tazobactam and Vancomycin | |
Cefepime, linezolid and Ciprofloxacin | |
Ciprofloxacin plus Meropenem | |
Azithromycin, Cefepime and Vancomycin |
Question 48 Explanation:
Either vancomycin or linezolid could be used due to the presence of 70% of S. aureus isolates being methicillin resistant. He also has a risk factor for multidrug-resistant pathogens due to being in the hospital for 5 days. Therefore, 2 antipseudomonal antibiotics would be used for empiric treatment. The antibiogram for the agents listed indicate that Pseudomonas aeruginosa are sensitive to these agents. An appropriate combination therapy would be cefepime, linezolid, and ciprofloxacin since there is coverage for MRSA and Pseudomonas aeruginosa.
Reference:
Kalil AC, Metersky ML, Klompas M, et al. Management of Adults With Hospital-acquired and Ventilator-associated Pneumonia: 2016 Clinical Practice Guidelines by the Infectious Diseases Society of America and the American Thoracic Society. Clin Infect Dis. 2016;ciw353. doi:10.1093/cid/ciw353.
Reference:
Kalil AC, Metersky ML, Klompas M, et al. Management of Adults With Hospital-acquired and Ventilator-associated Pneumonia: 2016 Clinical Practice Guidelines by the Infectious Diseases Society of America and the American Thoracic Society. Clin Infect Dis. 2016;ciw353. doi:10.1093/cid/ciw353.
Question 49 |
JM is a 66 YOM comes to your clinic complaining of excessive thirst and urination for the past one month. His past medical history includes hypertension and dyspepsia. Home medications includes amlodipine 5mg by mouth daily and famotidine 20 mg by mouth twice daily. He is 5 feet 8 inches and weighs 180 pounds. Point of care plasma glucose test was 224 mg/dl. His 2 average blood pressures are 124/78. Which of the following statements is true about JM’s diagnosis of type 2 diabetes(D2M)?
A1C must be above 6.5 % to diagnose him of D2M. | |
2 hours plasma glucose of ≥ 200mg/dl after a 75 gm oral glucose load must be done to diagnose him of D2M. | |
Fasting plasma glucose of ≥ 126 mg/dl must be obtained for a diagnosis of D2M. | |
JM already has a diagnosis of D2M based on his random plasma glucose of ≥ 200mg/dl and the presence of diabetes mellitus symptoms. |
Question 49 Explanation:
This patient’s symptoms of excessive thirst and urination over the past month plus random plasma glucose ≥ 200mg/dl gives him diagnosis for diabetes. Answer choices A, B, and C are also correct options for criteria to meet diagnosis for any patient, however they do not fit this patient specifically. Only one of these 4 criteria has to be met to meet diagnosis. The AACE/ACE 2015 guidelines defines possible symptoms of diabetes mellitus as frequent thirst (polydipsia), frequent urination (polyuria), polyphagia (extreme hunger), blurred vision, weakness, and unexplained weight loss.
Reference:
I. American Diabetes Association. In Standards of Medical Care in Diabetes 2016. Diabetes Care 2016;39(Suppl. 1)
II. Garber AJ, et al. Consensus Statement by the American Association of Clinical Endocrinologists and American College of Endocrinology on the Comprehensive Type 2 Diabetes Management Algorithm – 2016 Executive Summary. EndocrPract. 2016; 22(1):84-113
Reference:
I. American Diabetes Association. In Standards of Medical Care in Diabetes 2016. Diabetes Care 2016;39(Suppl. 1)
II. Garber AJ, et al. Consensus Statement by the American Association of Clinical Endocrinologists and American College of Endocrinology on the Comprehensive Type 2 Diabetes Management Algorithm – 2016 Executive Summary. EndocrPract. 2016; 22(1):84-113
Question 50 |
LD is a 67-year-old immunocompetent male who received PPSV23 when he was 63. His past medical history includes DM, HTN and COPD. Which of the following is the correct course of action in regards to pneumococcal vaccine?
Give him PPSV23 followed by PCV13 a year later. | |
Give him PCV13 followed by PPSV23 5 years after the last dose of PPSV23. | |
Give him PCV13 5 years after the last dose of PPSV23 | |
Give him PCV13 then he is done with her Pneumococcal vaccine |
Question 50 Explanation:
Adults aged 65 or older who are immunocompetent and who have not received PCV13 but who have 1 or more doses of PPSV23 at age <65 years administer PCV13 at least 1 year after the most recent dose of PPSV23, thus C is wrong. Then, administer a dose of PPSV23 at least 1 year after PCV13 and at least 5 years after the most recent dose of PPSV23, thus D is wrong. The interval between PPSV23 doses should be at least 5 years, thus A is wrong.
Reference:
I. Adult Immunization Schedule. Centers for Disease Control and Prevention. http://www.cdc.gov/vaccines/schedules/hcp/adult.html. Updated April 20, 2016. Accessed September 27, 2016
Reference:
I. Adult Immunization Schedule. Centers for Disease Control and Prevention. http://www.cdc.gov/vaccines/schedules/hcp/adult.html. Updated April 20, 2016. Accessed September 27, 2016
Question 51 |
SR is a 79 YOM resident of acute rehabilitation unit has a past medical history of Atrial fibrillation , sinusitis, renal failure on hemodialysis, CHF, COPD, MI, Anemia and dysphagia. His past surgical history includes Tonsillectomy, CABG, Maze procedure with ablation for atrial fibrillation and PEG tube placement. SR has NKDA and he weighs 65kg. His current medications includes, Albuterol/Ipratropium 0.5mg/3mg inhalation q6h, Acetylcysteine 20% 600mg Inhalation Q12H, Aspirin 81mg, Budesonide 0.5mg inhalation q12h, Bumetanide 2mg via peg tube daily, Ferrous sulfate 300mg via peg tube BID, Gabapentin 300mg via peg tube TID, Montelukast 10mg via peg tube daily, Multivitamin via peg tube daily, Pantoprazole 40mg via peg tube daily, Sotalol 80mg via peg BID, Zinc oxide topical to skin BID. Pertinent labs: BUN 47mg/dl, creatinine 2.8mg/dl, potassium 3.7mmol/L, creatinine clearance 22ml/min. Hgb 6.9g/dl, Hct 22.4%. BP 135/60 mm Hg, HR 67 beats/min. Pulse oximetry 94%. His electrocardiogram showed P-R interval 146, Ventricular Rate 60 beats per minute, QTc 562 milliseconds, Atrial Rate 60 beats per minute.
Pertaining to Sotatol what drug therapy modification needs to be made?
Discontinue Sotalol
| |
Change Sotalol to 80mg daily
| |
Change Sotalol to 160mg twice daily
| |
Make no changes. |
Question 51 Explanation:
The patient is currently taking Sotalol 80mg via peg BID. SR has a QTc of 562 msec. Since this is greater than 560 msec, Sotalol should be discontinued. This dose is also not appropriate since SR has renal failure and is on hemodialysis. He has a CrCl of 22 mL/min. For ventricular arrhythmias, Sotalol should be extended to every 36 to 48 hours according to clinical response. However, for atrial fibrillation, a CrCl of less than 40 mL/min is contraindicated. Therefore, Sotalol should be discontinued.
References:
I. Sotalol. In: Clinical Pharmacology [database on the Internet]. Tampa (FL): Gold Standard; 2016 [updated 9 June 2016; cited 27 Aug 2016]. Available from: www.clinicalpharmacology.com.
II. Sotylize (sotalol oral solution) package insert. Atalnta, GA: Arbor Pharmaceuticals, LLC; 2016 Aug
References:
I. Sotalol. In: Clinical Pharmacology [database on the Internet]. Tampa (FL): Gold Standard; 2016 [updated 9 June 2016; cited 27 Aug 2016]. Available from: www.clinicalpharmacology.com.
II. Sotylize (sotalol oral solution) package insert. Atalnta, GA: Arbor Pharmaceuticals, LLC; 2016 Aug
Question 52 |
SR is a 79 YOM resident of acute rehabilitation unit has a past medical history of atrial fibrillation , sinusitis, renal failure on hemodialysis, CHF, COPD, MI, anemia and dysphagia. His past surgical history includes Tonsillectomy, CABG, Maze procedure with ablation for atrial fibrillation and PEG tube placement. SR has NKDA and he weighs 65kg. His current medications includes, Albuterol/Ipratropium 0.5mg/3mg inhalation q6h, Acetylcysteine 20% 600mg Inhalation Q12H, Aspirin 81mg, Budesonide 0.5mg inhalation q12h, Bumetanide 2mg via peg tube daily, Ferrous sulfate 300mg via peg tube BID, Gabapentin 300mg via peg tube TID, Montelukast 10mg via peg tube daily, Multivitamin via peg tube daily, Pantoprazole 40mg via peg tube daily, Sotalol 80mg via peg BID, Zinc oxide topical to skin BID. Pertinent labs: BUN 47mg/dl, creatinine 2.8mg/dl, potassium 3.7mmol/L, creatinine clearance 22ml/min. Hgb 6.9g/dl, Hct 22.4%. BP 135/60 mm Hg, HR 67 beats/min. Pulse oximetry 94%. His electrocardiogram showed P-R interval 146, Ventricular Rate 60 beats per minute, QTc 562 milliseconds, atrial rate 60 beats per minute. What should be monitored in patients receiving Sotalol ?
Magnesium
| |
QTc
| |
Potassium
| |
All of the above |
Question 52 Explanation:
In patients receiving Sotalol, serum creatinine, magnesium, potassium, heart rate, blood pressure, and ECG (QTc interval) should be monitored. If the baseline QTc is greater than 450 msec, then sotalol use is contraindicated.
If the QTc is greater than or equal to 500 msec, then the dose should be reduced, interval prolonged, or discontinued. If the QTc is less than 500 msec after 3 days, then the patient may be discharged on the current regimen. QTc would be monitored periodically afterwards. Sotalol has the potential to cause life-threatening ventricular tachycardia associated with QT interval prolongation. The dosing interval should be adjusted based on CrCl since QTc prolongation is directly related to the concentration of sotalol. Having a reduced CrCl and reduced heart rate increases the risk for QTc prolongation and torsades de pointes. Other conditions that may increase the risk of QT prolongation include bradycardia, hypertension, hypomagnesemia, and hypokalemia. Potassium should be greater than 4
References:
Sotylize (sotalol oral solution) package insert. Atalnta, GA: Arbor Pharmaceuticals, LLC; 2016 Aug Sotalol. In: Clinical Pharmacology [database on the Internet]. Tampa (FL): Gold Standard; 2016 [updated 9 June 2016; cited 27 Aug 2016]. Available from: http://www.clinicalpharmacology.com
References:
Sotylize (sotalol oral solution) package insert. Atalnta, GA: Arbor Pharmaceuticals, LLC; 2016 Aug Sotalol. In: Clinical Pharmacology [database on the Internet]. Tampa (FL): Gold Standard; 2016 [updated 9 June 2016; cited 27 Aug 2016]. Available from: http://www.clinicalpharmacology.com
Question 53 |
SR is a 79 YOM resident of acute rehabilitation unit has a past medical history of Atrial fibrillation , sinusitis, renal failure on hemodialysis, CHF, COPD, MI, Anemia and dysphagia. His past surgical history includes Tonsillectomy, CABG, Maze procedure with ablation for atrial fibrillation and PEG tube placement. SR has NKDA and he weighs 65kg. His current medications includes, Albuterol/Ipratropium 0.5mg/3mg inhalation q6h, Acetylcysteine 20% 600mg Inhalation Q12H, Aspirin 81mg, Budesonide 0.5mg inhalation q12h, Bumetanide 2mg via peg tube daily, Ferrous sulfate 300mg via peg tube BID, Gabapentin 300mg via peg tube TID, Montelukast 10mg via peg tube daily, Multivitamin via peg tube daily, Pantoprazole 40mg via peg tube daily, Sotalol 80mg via peg BID, Zinc oxide topical to skin BID. Pertinent labs: BUN 47mg/dl, creatinine 2.8mg/dl, potassium 3.7mmol/L, creatinine clearance 22ml/min. Hgb 6.9g/dl, Hct 22.4%. BP 135/60 mm Hg, HR 67 beats/min. Pulse oximetry 94%. His electrocardiogram showed P-R interval 146, Ventricular Rate 60 beats per minute, QTc 562 milliseconds, Atrial Rate 60 beats per minute. What are the complications / side effects of using Pantoprazole?
Clostridium difficile-associated diarrhea
| |
Bone fractures
| |
Pneumonia
| |
All of the above |
Question 53 Explanation:
Therapy with PPI is also associated with an increased risk of enteric infections such as Clostridium difficile-associated diarrhea, bone fractures, pneumonia, nutritional deficiencies and interference with the metabolism of antiplatelet drugs. In older patients, overprescribing of a PPI is associated with increases in morbidity, adverse drug events, hospitalization, and mortality. These risks are possibly due to geriatric patients having a higher risk of experiencing adverse drug reactions, presence of multiple morbidities, and use of other medications.
References:
Heidelbaugh JJ, Kim AH, Chang R, Walker PC. Overutilization of proton-pump inhibitors: what the clinician needs to know. Therap Adv Gastroenterol. 2012;5(4):219-32. doi: 10.1177/1756283X12437358. Delcher A, Hily S, Boureau AS, Chapelet G, Berrut G, De decker L. Multimorbidities and Overprescription of Proton Pump Inhibitors in Older Patients. PLoS ONE. 2015;10(11):e0141779. doi: 10.1371/journal.pone.0141779.
References:
Heidelbaugh JJ, Kim AH, Chang R, Walker PC. Overutilization of proton-pump inhibitors: what the clinician needs to know. Therap Adv Gastroenterol. 2012;5(4):219-32. doi: 10.1177/1756283X12437358. Delcher A, Hily S, Boureau AS, Chapelet G, Berrut G, De decker L. Multimorbidities and Overprescription of Proton Pump Inhibitors in Older Patients. PLoS ONE. 2015;10(11):e0141779. doi: 10.1371/journal.pone.0141779.
Question 54 |
SR is a 79 YOM resident of acute rehabilitation unit has a past medical history of atrial fibrillation , sinusitis, renal failure on hemodialysis, CHF, COPD, MI, anemia and dysphagia. His past surgical history includes Tonsillectomy, CABG, Maze procedure with ablation for atrial fibrillation and PEG tube placement. SR has NKDA and he weighs 65kg. His current medications includes, Albuterol/Ipratropium 0.5mg/3mg inhalation q6h, Acetylcysteine 20% 600mg Inhalation Q12H, Aspirin 81mg, Budesonide 0.5mg inhalation q12h, Bumetanide 2mg via peg tube daily, Ferrous sulfate 300mg via peg tube BID, Gabapentin 300mg via peg tube TID, Montelukast 10mg via peg tube daily, Multivitamin via peg tube daily, Pantoprazole 40mg via peg tube daily, Sotalol 80mg via peg BID, Zinc oxide topical to skin BID. Pertinent labs: BUN 47mg/dl, creatinine 2.8mg/dl, potassium 3.7mmol/L, creatinine clearance 22ml/min. Hgb 6.9g/dl, Hct 22.4%. BP 135/60 mm Hg, HR 67 beats/min. Pulse oximetry 94%. His electrocardiogram showed P-R interval 146, ventricular rate 60 beats per minute, QTc 562 milliseconds, atrial rate 60 beats per minute. What is SR’s CHADS2-VASc score?
5
| |
4
| |
3
| |
2 |
Question 54 Explanation:
CHA2DS2-VASc: 4.
1 point each: Congestive heart failure, vascular disease (MI)
2 points: Age > 75 years (79 YO)
SR’s score is based off the amount of points assigned to each condition that increases his risk of stroke. He received two points for being 79 years of age. Two more points were given for his congestive heart failure and prior history of MI. Therefore, SR has a total score of 4.
Condition Score
Congestive heart failure 1
Hypertension 1
Age ≥ 75 y 2
Diabetes mellitus 1
Stroke/TIA/TE 2
Vascular disease (prior MI, PAD, or aortic plaque) 1
Aged 65 to 74 y 1
Sex category (ie, female) 1
Maximum score = 9
Reference:
Lane DA, Lip GY. Use of the CHA(2)DS(2)-VASc and HAS-BLED scores to aid decision making for thromboprophylaxis in nonvalvular atrial fibrillation. Circulation. 2012;126(7):860-5. doi: 10.1161/CIRCULATIONAHA.111.060061. Retrieved on Feb 8th, 2017 from: http://circ.ahajournals.org/content/126/7/860
Reference:
Lane DA, Lip GY. Use of the CHA(2)DS(2)-VASc and HAS-BLED scores to aid decision making for thromboprophylaxis in nonvalvular atrial fibrillation. Circulation. 2012;126(7):860-5. doi: 10.1161/CIRCULATIONAHA.111.060061. Retrieved on Feb 8th, 2017 from: http://circ.ahajournals.org/content/126/7/860
Question 55 |
SR is a 79 YOM resident of acute rehabilitation unit has a past medical history of Atrial fibrillation , sinusitis, renal failure on hemodialysis, CHF, COPD, MI, Anemia and dysphagia. His past surgical history includes Tonsillectomy, CABG, Maze procedure with ablation for atrial fibrillation and PEG tube placement. SR has NKDA and he weighs 65kg. His current medications includes, Albuterol/Ipratropium 0.5mg/3mg inhalation q6h, Acetylcysteine 20% 600mg Inhalation Q12H, Aspirin 81mg, Budesonide 0.5mg inhalation q12h, Bumetanide 2mg via peg tube daily, Ferrous sulfate 300mg via peg tube BID, Gabapentin 300mg via peg tube TID, Montelukast 10mg via peg tube daily, Multivitamin via peg tube daily, Pantoprazole 40mg via peg tube daily, Sotalol 80mg via peg BID, Zinc oxide topical to skin BID. Pertinent labs: BUN 47mg/dl, creatinine 2.8mg/dl, potassium 3.7mmol/L, creatinine clearance 22ml/min. Hgb 6.9g/dl, Hct 22.4%. BP 135/60 mm Hg, HR 67 beats/min. Pulse oximetry 94%. His electrocardiogram showed P-R interval 146, Ventricular Rate 60 beats per minute, QTc 562 milliseconds, Atrial Rate 60 beats per minute. Which of the following is true regarding initiating antithrombotic therapy in patients with A. Fib?
For CHA2DS2-VASc Score of 1, recommend antithrombotic therapy with oral anticoagulation or antiplatelet therapy but oral anticoagulant preferred.
| |
Recommend oral anticoagulation only in patients with CHA2DS2-VASc Score ≥ 2
| |
Recommend oral anticoagulation only in patients with CHA2DS2-VASc Score ≥ 3
| |
A and B. |
Question 55 Explanation:
CHA2DS2-VASc Score of 0: recommend no antithrombotic therapy. CHA2DS2-VASc Score of 1: recommend antithrombotic therapy with oral anticoagulation or antiplatelet therapy but oral anticoagulant preferred. CHA2DS2-VASc Score ≥ 2: recommend oral anticoagulation
Reference:
Lane DA, Lip GY. Use of the CHA(2)DS(2)-VASc and HAS-BLED scores to aid decision making for thromboprophylaxis in nonvalvular atrial fibrillation. Circulation. 2012;126(7):860-5. doi: 10.1161/CIRCULATIONAHA.111.060061. Retrieved on Feb 8th, 2017 from: http://circ.ahajournals.org/content/126/7/860
Reference:
Lane DA, Lip GY. Use of the CHA(2)DS(2)-VASc and HAS-BLED scores to aid decision making for thromboprophylaxis in nonvalvular atrial fibrillation. Circulation. 2012;126(7):860-5. doi: 10.1161/CIRCULATIONAHA.111.060061. Retrieved on Feb 8th, 2017 from: http://circ.ahajournals.org/content/126/7/860
Question 56 |
SR is a 79 YOM resident of acute rehabilitation unit has a past medical history of Atrial fibrillation , sinusitis, renal failure on hemodialysis, CHF, COPD, MI, Anemia and dysphagia. His past surgical history includes Tonsillectomy, CABG, Maze procedure with ablation for atrial fibrillation and PEG tube placement. SR has NKDA and he weighs 65kg. His current medications includes, Albuterol/Ipratropium 0.5mg/3mg inhalation q6h, Acetylcysteine 20% 600mg Inhalation Q12H, Aspirin 81mg, Budesonide 0.5mg inhalation q12h, Bumetanide 2mg via peg tube daily, Ferrous sulfate 300mg via peg tube BID, Gabapentin 300mg via peg tube TID, Montelukast 10mg via peg tube daily, Multivitamin via peg tube daily, Pantoprazole 40mg via peg tube daily, Sotalol 80mg via peg BID, Zinc oxide topical to skin BID. Pertinent labs: BUN 47mg/dl, creatinine 2.8mg/dl, potassium 3.7mmol/L, creatinine clearance 22ml/min. Hgb 6.9g/dl, Hct 22.4%. BP 135/60 mm Hg, HR 67 beats/min. Pulse oximetry 94%. His electrocardiogram showed P-R interval 146, Ventricular Rate 60 beats per minute, QTc 562 milliseconds, Atrial Rate 60 beats per minute. What is SR’s HAS-BLED scores?
2
| |
3
| |
4
| |
5 |
Question 56 Explanation:
HAS-BLED: 4.
1 point each: Elderly (age > 65 y), bleeding tendency/predisposition, drugs, and abnormal renal function
SR has a HAS-BLED score of 4. SR is 79 years old. He has abnormal renal function due to renal failure on hemodialysis with a serum creatinine > 200 mmol/L, has a history of anemia, and is taking aspirin. These conditions are considered bleeding risk factors. Since SR has a score of 4, he is at a high risk for bleeding. Scores greater than or equal to 3 indicate a high risk for bleeding. Caution with treatment and regular review of the patient is recommended due to this score.
Condition Score Hypertension (systolic blood pressure > 160 mm Hg) 1 Abnormal renal or liver function (1 point each) 1 or 2 Stroke 1 Bleeding tendency/predisposition 1 Labile INRs (if on warfarin) 1 Elderly (eg, age > 65 y) 1 Drugs or alcohol (1 point each) 1 or 2 Maximum score = 9 HAS-BLED Score of 0 or 1: low risk of bleeding. HAS-BLED Score of 2: intermediate risk of bleeding. HAS-BLED Score of ≥ 3: high risk of bleeding (indicates that caution is warranted when prescribing oral anticoagulation and regular review is recommended)
Reference:
Lane DA, Lip GY. Use of the CHA(2)DS(2)-VASc and HAS-BLED scores to aid decision making for thromboprophylaxis in nonvalvular atrial fibrillation. Circulation. 2012;126(7):860-5. doi: 10.1161/CIRCULATIONAHA.111.060061. Retrieved on Feb 8th, 2017 from: http://circ.ahajournals.org/content/126/7/860
SR has a HAS-BLED score of 4. SR is 79 years old. He has abnormal renal function due to renal failure on hemodialysis with a serum creatinine > 200 mmol/L, has a history of anemia, and is taking aspirin. These conditions are considered bleeding risk factors. Since SR has a score of 4, he is at a high risk for bleeding. Scores greater than or equal to 3 indicate a high risk for bleeding. Caution with treatment and regular review of the patient is recommended due to this score.
Condition Score Hypertension (systolic blood pressure > 160 mm Hg) 1 Abnormal renal or liver function (1 point each) 1 or 2 Stroke 1 Bleeding tendency/predisposition 1 Labile INRs (if on warfarin) 1 Elderly (eg, age > 65 y) 1 Drugs or alcohol (1 point each) 1 or 2 Maximum score = 9 HAS-BLED Score of 0 or 1: low risk of bleeding. HAS-BLED Score of 2: intermediate risk of bleeding. HAS-BLED Score of ≥ 3: high risk of bleeding (indicates that caution is warranted when prescribing oral anticoagulation and regular review is recommended)
Reference:
Lane DA, Lip GY. Use of the CHA(2)DS(2)-VASc and HAS-BLED scores to aid decision making for thromboprophylaxis in nonvalvular atrial fibrillation. Circulation. 2012;126(7):860-5. doi: 10.1161/CIRCULATIONAHA.111.060061. Retrieved on Feb 8th, 2017 from: http://circ.ahajournals.org/content/126/7/860
Question 57 |
SR is a 79 YOM resident of acute rehabilitation unit has a past medical history of Atrial fibrillation , sinusitis, renal failure on hemodialysis, CHF, COPD, MI, Anemia and dysphagia. His past surgical history includes Tonsillectomy, CABG, Maze procedure with ablation for atrial fibrillation and PEG tube placement. SR has NKDA and he weighs 65kg. His current medications includes, Albuterol/Ipratropium 0.5mg/3mg inhalation q6h, Acetylcysteine 20% 600mg Inhalation Q12H, Aspirin 81mg, Budesonide 0.5mg inhalation q12h, Bumetanide 2mg via peg tube daily, Ferrous sulfate 300mg via peg tube BID, Gabapentin 300mg via peg tube TID, Montelukast 10mg via peg tube daily, Multivitamin via peg tube daily, Pantoprazole 40mg via peg tube daily, Sotalol 80mg via peg BID, Zinc oxide topical to skin BID. Pertinent labs: BUN 47mg/dl, creatinine 2.8mg/dl, potassium 3.7mmol/L, creatinine clearance 22ml/min. Hgb 6.9g/dl, Hct 22.4%. BP 135/60 mm Hg, HR 67 beats/min. Pulse oximetry 94%. His electrocardiogram showed P-R interval 146, Ventricular Rate 60 beats per minute, QTc 562 milliseconds, Atrial Rate 60 beats per minute. What is the indication for Acetylcysteine 20% 600mg inhalation q12h for SR?
For acetaminophen overdose given via inhalation
| |
For prevention of contrast-induced nephropathy
| |
As a mucolytic agent to decreases mucus viscosity
| |
As an antiseptic to prevent pneumonia |
Question 57 Explanation:
The indication for Acetylcysteine 20% 600mg inhalation q12h is an adjunct to the treatment of his COPD as a mucolytic. Indications: Acetaminophen overdose, amyloidosis, bronchiectasis, chronic bronchitis, COPD, emphysema, mucolytic off label: Prevention of contrast-induced nephropathy, distal intestinal obstruction syndrome (DIOS), giant papillary conjunctivitis (GPC). MOA: As a mucolytic, the free sulfhydryl groups in acetylcysteine are believed to open up the disulfide bonds of the mucoproteins in bronchial secretions, which results in decreased hypersecretion and mucous viscosity of the lungs. This also helps in the removal of secretions through coughing, mechanical mechanisms, or postural drainage.
References:
Acetylcysteine. In: Clinical Pharmacology [database on the Internet]. Tampa (FL): Gold Standard; 2016 [updated 2 Aug 2016; cited 26 Aug 2016]. Available from: www.clinicalpharmacology.com
References:
Acetylcysteine. In: Clinical Pharmacology [database on the Internet]. Tampa (FL): Gold Standard; 2016 [updated 2 Aug 2016; cited 26 Aug 2016]. Available from: www.clinicalpharmacology.com
Question 58 |
SR is a 79 YOM resident of acute rehabilitation unit has a past medical history of Atrial fibrillation , sinusitis, renal failure on hemodialysis, CHF, COPD, MI, Anemia and dysphagia. His past surgical history includes Tonsillectomy, CABG, Maze procedure with ablation for atrial fibrillation and PEG tube placement. SR has NKDA and he weighs 65kg. His current medications includes, Albuterol/Ipratropium 0.5mg/3mg inhalation q6h, Acetylcysteine 20% 600mg Inhalation Q12H, Aspirin 81mg, Budesonide 0.5mg inhalation q12h, Bumetanide 2mg via peg tube daily, Ferrous sulfate 300mg via peg tube BID, Gabapentin 300mg via peg tube TID, Montelukast 10mg via peg tube daily, Multivitamin via peg tube daily, Pantoprazole 40mg via peg tube daily, Sotalol 80mg via peg BID, Zinc oxide topical to skin BID. Pertinent labs: BUN 47mg/dl, creatinine 2.8mg/dl, potassium 3.7mmol/L, creatinine clearance 22ml/min. Hgb 6.9g/dl, Hct 22.4%. BP 135/60 mm Hg, HR 67 beats/min. Pulse oximetry 94%. His electrocardiogram showed P-R interval 146, Ventricular Rate 60 beats per minute, QTc 562 milliseconds, Atrial Rate 60 beats per minute. What electrolytes abnormality is/are commonly seen with the administration of bumetanide?
Hyponatremia
| |
Hypokalemia
| |
Hypochloremia
| |
All of the above |
Question 58 Explanation:
The electrolytes that should be closely monitored in patients taking bumetanide include potassium, sodium, chloride, calcium, magnesium, bicarbonate, ammonium, and phosphate. Electrolyte abnormalities reported during bumetanide therapy have included hypochloremia (14.9%), hypokalemia (14.7%), and hyponatremia (9.2%). Bumetanide may also increase urinary calcium and phosphate excretion with resultant hypocalcemia and/or hypophosphatemia. Bumetanide is a potent diuretic with a Boxed Warning of fluid/electrolyte loss. If given in excess, profound diuresis with water and electrolyte depletion may occur. Loss of these electrolytes may lead to metabolic alkalosis. This can be treated with potassium chloride replacement. Other concerns include serious cardiac arrhythmias that may occur due to the electrolyte disturbances.
References:
Bumetanide. In: Clinical Pharmacology [database on the Internet]. Tampa (FL): Gold Standard; 2016 [updated 1 July 2015; cited 26 Aug 2016]. Available from: www.clinicalpharmacology.com.
References:
Bumetanide. In: Clinical Pharmacology [database on the Internet]. Tampa (FL): Gold Standard; 2016 [updated 1 July 2015; cited 26 Aug 2016]. Available from: www.clinicalpharmacology.com.
Question 59 |
SR is a 79 YOM resident of acute rehabilitation unit has a past medical history of atrial fibrillation , sinusitis, renal failure on hemodialysis, CHF, COPD, MI, anemia and dysphagia. His past surgical history includes tonsillectomy, CABG, Maze procedure with ablation for atrial fibrillation and PEG tube placement. SR has NKDA and he weighs 65kg. His current medications includes, Albuterol/Ipratropium 0.5mg/3mg inhalation q6h, Acetylcysteine 20% 600mg Inhalation Q12H, Aspirin 81mg, Budesonide 0.5mg inhalation q12h, Bumetanide 2mg via peg tube daily, Ferrous sulfate 300mg via peg tube BID, Gabapentin 300mg via peg tube TID, Montelukast 10mg via peg tube daily, Multivitamin via peg tube daily, Pantoprazole 40mg via peg tube daily, Sotalol 80mg via peg BID, Zinc oxide topical to skin BID. Pertinent labs: BUN 47mg/dl, creatinine 2.8mg/dl, potassium 3.7mmol/L, creatinine clearance 22ml/min. Hgb 6.9g/dl, Hct 22.4%. BP 135/60 mm Hg, HR 67 beats/min. Pulse oximetry 94%. His electrocardiogram showed P-R interval 146, Ventricular Rate 60 beats per minute, QTc 562 milliseconds, atrial rate 60 beats per minute. What is the best treatment option for his chronic anemia due to renal failure?
Epoetin Alfa 3000 units subcutaneously 3 times a week.
| |
Epoetin 10000 units subcutaneously 3 times a week.
| |
Darbepoetin Alfa 200mcg subcutaneously every week.
| |
Blood transfusion |
Question 59 Explanation:
Epoetin Alfa should be initiated at 50 units/kg IV (or SubQ) 3 times a week for chronic anemia. This would be given due to his hemoglobin being at 6.9. Treatment would stop when his hemoglobin approaches 11 g/dL. Erythropoiesis-stimulating agents have been approved for the treatment of anemia in patients with chronic kidney disease who are undergoing hemodialysis to maintain a hemoglobin level of 10 to 11 g/dL. In patients with CHF with moderate to severe anemia (Hgb < 11 g/dL) and concomitant moderate to severe chronic kidney disease, guidelines of the National Kidney Foundation recommend treatment with erythropoietic agents and supplemental iron. For patients with CKD on dialysis the dose of Darbepoetin Alfa is 0.45 mcg/kg IV or subcutaneously once a week or 0.75 mcg/kg once every 2 weeks as appropriate. Blood transfusion is indicated in patients with acute anemia due to blood loss.
References:
I. National Kidney Foundation. KDOQI Clinical practice guidelines and recommendations for anemia of chronic kidney disease. Am J Kidney Dis 2006;47(suppl 3):S1-S146. Available at www.kidney.org/professionals/kdoqi/guidelines_anemia/ pdf/AnemiaInCKD.pdf. Accessed November 24, 2016.
II. Tang YD, Katz SD. Anemia in chronic heart failure: prevalence, etiology, clinical correlates, and treatment options. Circulation. 2006;113(20):2454-61.
III. Voak D, Chapman JF, and Phillips P. Quality of transfusion practice beyond the blood transfusion laboratory is essential to prevent ABO-incompatible death. Transfusion Medicine, 2000; 10: 95-96.
References:
I. National Kidney Foundation. KDOQI Clinical practice guidelines and recommendations for anemia of chronic kidney disease. Am J Kidney Dis 2006;47(suppl 3):S1-S146. Available at www.kidney.org/professionals/kdoqi/guidelines_anemia/ pdf/AnemiaInCKD.pdf. Accessed November 24, 2016.
II. Tang YD, Katz SD. Anemia in chronic heart failure: prevalence, etiology, clinical correlates, and treatment options. Circulation. 2006;113(20):2454-61.
III. Voak D, Chapman JF, and Phillips P. Quality of transfusion practice beyond the blood transfusion laboratory is essential to prevent ABO-incompatible death. Transfusion Medicine, 2000; 10: 95-96.
Question 60 |
SR is a 79 YOM resident of acute rehabilitation unit has a past medical history of atrial fibrillation , sinusitis, renal failure on hemodialysis, CHF, COPD, MI, anemia and dysphagia. His past surgical history includes Tonsillectomy, CABG, Maze procedure with ablation for atrial fibrillation and PEG tube placement. SR has NKDA and he weighs 65kg. His current medications includes, Albuterol/Ipratropium 0.5mg/3mg inhalation q6h, Acetylcysteine 20% 600mg Inhalation Q12H, Aspirin 81mg, Budesonide 0.5mg inhalation q12h, Bumetanide 2mg via peg tube daily, Ferrous sulfate 300mg via peg tube BID, Gabapentin 300mg via peg tube TID, Montelukast 10mg via peg tube daily, Multivitamin via peg tube daily, Pantoprazole 40mg via peg tube daily, Sotalol 80mg via peg BID, Zinc oxide topical to skin BID. Pertinent labs: BUN 47mg/dl, creatinine 2.8mg/dl, potassium 3.7mmol/L, creatinine clearance 22ml/min. Hgb 6.9g/dl, Hct 22.4%. BP 135/60 mm Hg, HR 67 beats/min. Pulse oximetry 94%. His electrocardiogram showed P-R interval 146, Ventricular Rate 60 beats per minute, QTc 562 milliseconds, atrial rate 60 beats per minute. Which of the following renal changes does not occur as the body ages?
Increase in total body water
| |
Decrease in renal mass
| |
Decrease in renal blood flow
| |
Decrease glomerular filtration rate |
Question 60 Explanation:
There is a progressive reduction in total body water and lean body mass that occurs and which results in a relative increase in body fat. Renal mass decreases with age and reflects the reduction in nephrons. Both renal plasma flow and as well as glomerular filtration rate decline with age.
Reference:
I. Mangoni AJackson S. Age-related changes in pharmacokinetics and pharmacodynamics: basic principles and practical applications. British Journal of Clinical Pharmacology. 2003;57(1):6-14. doi:10.1046/j.1365-2125.2003.02007.x. II. Summary of the Updated American Geriatrics Society/British Geriatrics Society clinical practice guideline for prevention of falls in older persons. J Am Geriatr Soc 2011;59:148-57. Available at: http://www.americangeriatrics.org/files/documents/health_care_pros/JAGS.Falls.Guidelines.pdf
Reference:
I. Mangoni AJackson S. Age-related changes in pharmacokinetics and pharmacodynamics: basic principles and practical applications. British Journal of Clinical Pharmacology. 2003;57(1):6-14. doi:10.1046/j.1365-2125.2003.02007.x. II. Summary of the Updated American Geriatrics Society/British Geriatrics Society clinical practice guideline for prevention of falls in older persons. J Am Geriatr Soc 2011;59:148-57. Available at: http://www.americangeriatrics.org/files/documents/health_care_pros/JAGS.Falls.Guidelines.pdf
Question 61 |
Which of the following pulmonary changes is/are seen as body ages?
Decrease in expiratory flow rate
| |
Decrease in vital capacity
| |
Decrease in respiratory muscle strength
| |
All of the above changes are seen a body ages |
Question 61 Explanation:
Expiratory flow rates decrease with aging and typically show changes in the flow-volume curves. Other age-related changes that occur in the lungs include weakening of the respiratory muscles as well as a decrease in lung measures of lung function such as vital capacity, which is the maximum amount of air that can be breathed out following a maximum inhalation.
Reference:
I. Janssens J, Pache J, Nicod L. Physiological changes in respiratory function associated with ageing. European Respiratory Journal. 1999;13(1):197-205. Available at: http://erj.ersjournals.com/content/13/1/197.long. , /a> Accessed October 13, 2016.
II. System E. Effects of Aging on the Respiratory System. Merck Manuals Consumer Version. 2016. Available at: https://www.merckmanuals.com/home/lung-and-airway-disorders/biology-of-the-lungs-and-airways/effects-of-aging-on-the-respiratory-system.,/a> Accessed October 13, 2016.
Reference:
I. Janssens J, Pache J, Nicod L. Physiological changes in respiratory function associated with ageing. European Respiratory Journal. 1999;13(1):197-205. Available at: http://erj.ersjournals.com/content/13/1/197.long. , /a> Accessed October 13, 2016.
II. System E. Effects of Aging on the Respiratory System. Merck Manuals Consumer Version. 2016. Available at: https://www.merckmanuals.com/home/lung-and-airway-disorders/biology-of-the-lungs-and-airways/effects-of-aging-on-the-respiratory-system.,/a> Accessed October 13, 2016.
Question 62 |
Which of the following beta-blocker is NOT proven to reduce mortality in patients with Systolic CHF?
Bisoprolol
| |
Nadolol
| |
Carvedilol
| |
Metoprolol succinate |
Question 62 Explanation:
Nadolol is not proven to reduce mortality in patients with systolic CHF. The efficacy of nadolol in HF has not been determined. For patients taking nadolol, it should be used with caution in those with compensated heart failure and patients should be monitored for a worsening of the condition.
Bisoprolol, carvedilol, and sustained-release metoprolol succinate are the beta-blockers that have been proven to reduce mortality in patients with systolic CHF. These 3 beta-blockers have been effective in reducing the risk of death in patients with chronic HFrEF. Other beta-blockers were found to be less effective. Bucindolol did not exhibit uniform effectiveness across different populations. Metoprolol tartrate was found to be less effective in HF clinical trials.
References:
Yancy CW, Jessup M, Bozkurt B, et al. 2013 ACCF/AHA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines.J Am Coll Cardiol. 2013;62(16):e147-e239. doi:10.1016/j.jacc.2013.05.019. Retirved on Feb 6th from : http://circ.ahajournals.org/content/128/16/e240
References:
Yancy CW, Jessup M, Bozkurt B, et al. 2013 ACCF/AHA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines.J Am Coll Cardiol. 2013;62(16):e147-e239. doi:10.1016/j.jacc.2013.05.019. Retirved on Feb 6th from : http://circ.ahajournals.org/content/128/16/e240
Question 63 |
TM is a 78 YOW with a history of hypertension, hypercholesterolemia and arthritis was admitted for proximal atrial fibrillation. While in the hospital she was placed on diltiazem drip and eventually, converted to oral diltiazem 240mg. Pt’s home medications includes simvastatin 40mg po daily , hydrochlorothiazide 25mg po daily , lisinopril 20mg daily, and acetaminophen. Her LDL-C is 100mg /dL. What would be the most appropriate change to make on her therapy?
Increase simvastatin to 80mg po daily
| |
Keep simvastatin at 40mg po daily | |
Change simvastatin 40mg to atorvastatin 40mg po daily
| |
Change simvastatin to lovastatin 20mg po daily |
Question 63 Explanation:
Diltiazem has a major drug interaction with Simvastatin. Diltiazem is a CYP3A4 inhibitor, and since Simvastatin is metabolized by CYP3A4, its level can build up and the risk of myopathy increases. It is recommended to switch to a non-CYP3A inhibitor such as Pitavastatin, Pravastatin, or Rosuvastatin, and if Simvastatin is to be kept on it should not exceed 10 mg/day. The same interaction also exists with lovastatin, and the recommendation is to not exceed a total dose of 20 mg/day po of Lovastatin. Given the current options, the best choice is to change to Atorvstatin 40 mg po daily.
Reference:
I. FDA Drug Safety Communication: New restrictions, contraindications, and dose limitations for Zocor (simvastatin) to reduce the risk of muscle injury. December 15, 2011. Retrieved on Feb 8th, 2017 from : http://www.fda.gov/Drugs/DrugSafety/ucm256581.htm
II. Stone N, Robinson J, Lichtenstein A et al. 2013 ACC/AHA Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults. Circulation. 2013;129(25 suppl 2):S1-S45. doi:10.1161/01.cir.0000437738.63853.7a. Retrieved on Feb 6th 2017 from : http://circ.ahajournals.org/content/129/25_suppl_2/S1
Reference:
I. FDA Drug Safety Communication: New restrictions, contraindications, and dose limitations for Zocor (simvastatin) to reduce the risk of muscle injury. December 15, 2011. Retrieved on Feb 8th, 2017 from : http://www.fda.gov/Drugs/DrugSafety/ucm256581.htm
II. Stone N, Robinson J, Lichtenstein A et al. 2013 ACC/AHA Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults. Circulation. 2013;129(25 suppl 2):S1-S45. doi:10.1161/01.cir.0000437738.63853.7a. Retrieved on Feb 6th 2017 from : http://circ.ahajournals.org/content/129/25_suppl_2/S1
Question 64 |
What is the optimal duration of antibiotic therapy for HAP and VAP?
5 days
| |
7 days
| |
10 days
| |
14 days |
Question 64 Explanation:
Short-course antibiotic therapy is associated with less antibiotic exposure and antibiotic resistance. This would result in reduced costs and side effects. The benefits of therapy are not reduced with a shorter duration.
Reference:
Kalil AC, Metersky ML, Klompas M, et al. Management of Adults With Hospital-acquired and Ventilator-associated Pneumonia: 2016 Clinical Practice Guidelines by the Infectious Diseases Society of America and the American Thoracic Society. Clin Infect Dis. 2016;ciw353. doi:10.1093/cid/ciw353. Retrieved on feb 8th, 2017 from : https://academic.oup.com/cid/article/63/5/e61/2237650/Management-of-Adults-With-Hospital-acquired-and
Reference:
Kalil AC, Metersky ML, Klompas M, et al. Management of Adults With Hospital-acquired and Ventilator-associated Pneumonia: 2016 Clinical Practice Guidelines by the Infectious Diseases Society of America and the American Thoracic Society. Clin Infect Dis. 2016;ciw353. doi:10.1093/cid/ciw353. Retrieved on feb 8th, 2017 from : https://academic.oup.com/cid/article/63/5/e61/2237650/Management-of-Adults-With-Hospital-acquired-and
Question 65 |
PM is a 69 YOM who has never received the zoster vaccine. When he was 57 years old he had an episode of herpes zoster. He wants to know if he is a candidate for the zoster vaccine. Which of the following statements is true?
No he is not a candidate for zoster vaccine since he already had herpes zoster and has built immunity to it.
| |
Yes he is still candidate for zoster vaccine regardless of his prior episode of herpes zoster.
| |
No he is not a candidate since it is only indicated for patients who are under 60 years of age. | |
No he is not a candidate since it is only indicated for patients who are under 60 years of age. |
Question 65 Explanation:
A single dose of zoster vaccine is recommended for all adults 60 years or older, regardless of whether they report a prior episode of herpes zoster, thus A is wrong. Also, although 2nd and 3rd episodes of herpes zoster can occur, the annual incidence of recurrence is not known. Although the FDA recommends the administration of the vaccine for individuals 50 years or older, the ACIP recommends that vaccinations begin at 60 years, thus C and D are incorrect.
Reference:
I. Shingles | Clinical Overview - Varicella Vaccine | Herpes Zoster | CDC. Cdcgov. 2016. Available at: http://www.cdc.gov/shingles/hcp/clinical-overview.html. Accessed September 27, 2016.
II. Adult Immunization Schedule. Centers for Disease Control and Prevention. http://www.cdc.gov/vaccines/schedules/hcp/adult.html. Updated April 20, 2016. Accessed September 27, 2016
Reference:
I. Shingles | Clinical Overview - Varicella Vaccine | Herpes Zoster | CDC. Cdcgov. 2016. Available at: http://www.cdc.gov/shingles/hcp/clinical-overview.html. Accessed September 27, 2016.
II. Adult Immunization Schedule. Centers for Disease Control and Prevention. http://www.cdc.gov/vaccines/schedules/hcp/adult.html. Updated April 20, 2016. Accessed September 27, 2016
Question 66 |
JP 77 YOWM with a history of hypertension was recently admitted for ischemic stroke. What would be the most appropriate pharmacotherapy recommendation upon discharge?
Aorvastatin 20 mg PO QHS
| |
Pitavastatin 1 mg PO QHS
| |
Atorvastatin 80 mg PO QHS
| |
Lovastatin 20 mg PO QHS |
Question 66 Explanation:
A stroke falls under the category of clinical ASCVD, which includes includes acute coronary syndromes, or a history of MI, stable or unstable angina, coronary or other arterial revascularization, stroke, TIA, or peripheral arterial disease presumed to be of atherosclerotic origin. Patients with clinical ASCVD are at an increased risk for recurrent ASCVD and ASCVD death. This patient is over 75 years old, and such patients with clinical ASCVD should receive moderate-intensity statin therapy. However, ATP4 acknowledges that the older patients in the corresponding RCTs were likely to be healthier than those in the general population, so treatment can be individualized. Given the options above, a high intensity statin is the most appropriate option. The decision to start at the 80 mg dose of atorvastatin instead of the 40 mg dose is based on the recommendation to down titrate if the patient is unable to tolerate the 80 mg dose as opposed to up-titrating in accordance with the IDEAL trial.
Reference:
Stone N, Robinson J, Lichtenstein A et al. 2013 ACC/AHA Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults. Circulation. 2013;129(25 suppl 2):S1-S45. doi:10.1161/01.cir.0000437738.63853.7a. Retrieved on Feb 6th 2017 from : http://circ.ahajournals.org/content/129/25_suppl_2/S1
Reference:
Stone N, Robinson J, Lichtenstein A et al. 2013 ACC/AHA Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults. Circulation. 2013;129(25 suppl 2):S1-S45. doi:10.1161/01.cir.0000437738.63853.7a. Retrieved on Feb 6th 2017 from : http://circ.ahajournals.org/content/129/25_suppl_2/S1
Question 67 |
For what reason/s is it recommended to avoid benzodiazepine in elderly patients?
Increased risk of cognitive impairment
| |
Falls, fracture and motor vehicle crashes
| |
Delirium
| |
All of the above |
Question 67 Explanation:
In Table 3, all these conditions are reasons to avoid benzodiazepines. These medications affect the CNS and the elderly population can be more sensitive. With benzodiazepines having a depressant effect on the CNS it makes since that patients may be at risk for these conditions since the patient’s balance, reaction time, and cognitive abilities would be reduced.
Reference:
Radcliff, Sue, et al. "American Geriatrics Society 2015 updated beers criteria for potentially inappropriate medication use in older adults." JOURNAL OF THE AMERICAN GERIATRICS SOCIETY 63.11 (2015): 2227-2246. Available at: http://onlinelibrary.wiley.com/doi/10.1111/jgs.13702/full
Reference:
Radcliff, Sue, et al. "American Geriatrics Society 2015 updated beers criteria for potentially inappropriate medication use in older adults." JOURNAL OF THE AMERICAN GERIATRICS SOCIETY 63.11 (2015): 2227-2246. Available at: http://onlinelibrary.wiley.com/doi/10.1111/jgs.13702/full
Question 68 |
DM is a 75 YOW with a history of systolic heart failure who presents to the ER with a 5 day history of progressive worsening of shortness of breath. Her pro-B-Natriuretic Peptide is 28869 pg/ml, chest x-ray shows: cardiomegaly with pulmonary vascular congestion and atelectatic changes in the left mid lung. Bilateral pleural effusions. No chills or fevers. Her 2 average BP is 135/92, HR 72. Current medications are enalapril 20mg oral daily and carvedilol 6.5mg orally twice daily. Which of the following would be the immediate course of action?
Give normal saline at 100mls/hr
| |
Lasix 40mg intravenously twice daily and monitor fluid status
| |
Increase enalapril to 40mg oral twice daily
| |
Increase carvediolol to 25mg orally twice daily
Give normal saline at 100mls/hr |
Question 68 Explanation:
Initiating Lasix 40 mg IV twice daily would be the immediate course of action in order to improve symptoms of fluid retention. Fluid status would be monitored.Normal saline would not be given. DM would most likely have fluid restricted (1.5 to 2 L per day) to reduce congestive symptoms. For enalapril, the max dose is 20 BID for the treatment of heart failure. Increasing Enalapril would not improve symptoms of heart failure in the short term. Carvedilol would not be increased until after the patient is stable and IV diuretics stopped as well as any vasodilators and inotropic agents.
Reference
Yancy CW, Jessup M, Bozkurt B, et al. 2013 ACCF/AHA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines.J Am Coll Cardiol. 2013;62(16):e147-e239. doi:10.1016/j.jacc.2013.05.019. Retirved on Feb 6th from : http://circ.ahajournals.org/content/128/16/e240/
Reference
Yancy CW, Jessup M, Bozkurt B, et al. 2013 ACCF/AHA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines.J Am Coll Cardiol. 2013;62(16):e147-e239. doi:10.1016/j.jacc.2013.05.019. Retirved on Feb 6th from : http://circ.ahajournals.org/content/128/16/e240/
Question 69 |
DM is a 75 YOW with a history of systolic heart failure who presents to the ER with a 5 day history of progressive worsening of shortness of breath. Her pro-B-Natriuretic Peptide is 28869 pg/ml, chest x-ray shows: cardiomegaly with pulmonary vascular congestion and atelectatic changes in the left mid lung. Bilateral pleural effusions. No chills or fevers. Her 2 average BP is 135/92, HR 72. Current medication are enalapril 20mg oral daily and carvedilol 6.5mg orally twice daily.
Four days later DM is on max dose of furosemide of 120mg iv q12h and metolazone 10mg daily, despite these diuretics her chest x-ray still shows pulmonary edema, her urine output has decreased, now she requires more oxygen, her creatinine clearance has gone up to 3.0. Which of the following medications would be most appropriate to initiate when DM is maxed out on diuretics?
Sodium nitroprussside
| |
Dobutamine
| |
Nitroglycerin
| |
Nesiritide |
Question 69 Explanation:
Nitroglycerin would be the most appropriate to initiate when DM is maxed out on diuretics. IV nitroglycerin helps to rapidly reduce pulmonary congestion. There is also no dosage adjustments provided for renal impairment.
Sodium nitroprusside can also dilate pulmonary vasculature. However, in patients with renal impairment, there is a risk of thiocyanate accumulation and toxicity. Nesiritide has a longer half-life compared to nitroglycerin and nitroprusside and may result in adverse effects occurring for a longer period of time, such as hypotension. Studies have also indicated that patients may be at risk for worsening renal function and increased mortality while taking nesiritide. A recent meta-analysis indicated that there was no significant increase in mortality. When compared to placebo, there was no increased risk of mortality in those treated with nesiritide. However, it is associated with an increased risk of cardiovascular adverse events such as bradycardia and hypotension. Dobutamine would not be used in this case. It would be used as short-term management in those with cardiac decompensation in order to maintain perfusion and preserve end-organ performance in those with cardiogenic shock; bridge therapy in those with stage D heart failure who are unresponsive to guideline-directed medical therapy and device therapy awaiting a heart transplant or mechanical circulatory support; treat those with severe systolic dysfunction who present with low blood pressure and significantly depressed cardiac output, or to provide palliative therapy in select patients. The guidelines also stated that intermittent IV positive inotropic therapy has no proven value in patients with stage C heart failure.
Reference
I. Yancy CW, Jessup M, Bozkurt B, et al. 2013 ACCF/AHA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines.J Am Coll Cardiol. 2013;62(16):e147-e239. doi:10.1016/j.jacc.2013.05.019. Retirved on Feb 6th from : http://circ.ahajournals.org/content/128/16/e240
II. Nesiritide. In: Clinical Pharmacology [database on the Internet]. Tampa (FL): Gold Standard; 2016 [updated 2 Aug 2010; cited 2 Sept 2016]. Available from: www.clinicalpharmacology.com
III. Gong B, Wu Z, Li Z. Efficacy and safety of nesiritide in patients with decompensated heart failure: a meta-analysis of randomised trials. BMJ Open. 2016;6(1):e008545. doi: 10.1136/bmjopen-2015-008545.
Reference
I. Yancy CW, Jessup M, Bozkurt B, et al. 2013 ACCF/AHA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines.J Am Coll Cardiol. 2013;62(16):e147-e239. doi:10.1016/j.jacc.2013.05.019. Retirved on Feb 6th from : http://circ.ahajournals.org/content/128/16/e240
II. Nesiritide. In: Clinical Pharmacology [database on the Internet]. Tampa (FL): Gold Standard; 2016 [updated 2 Aug 2010; cited 2 Sept 2016]. Available from: www.clinicalpharmacology.com
III. Gong B, Wu Z, Li Z. Efficacy and safety of nesiritide in patients with decompensated heart failure: a meta-analysis of randomised trials. BMJ Open. 2016;6(1):e008545. doi: 10.1136/bmjopen-2015-008545.
Question 70 |
DM is a 75 YOW with a history of systolic heart failure who presents to the ER with a 5 day history of progressive worsening of shortness of breath. Her pro-B-Natriuretic Peptide is 28869 pg/ml, chest x-ray shows: cardiomegaly with pulmonary vascular congestion and atelectatic changes in the left mid lung. Bilateral pleural effusions. No chills or fevers. Her 2 average BP is 135/92, HR 72. Current medication are enalapril 20mg oral daily and carvedilol 6.5mg orally twice daily.
An echocardiogram was ordered and her ejection fraction was estimated in the range of 25-30%. DM feels much better her SOB is improved. Her 2 average BP is 142/92, HR 72. All the diuretics have been stopped. Her hemodynamics are stable. What would be the next appropriate course of action?
Increase the carvedilol to 12.5mg orally twice daily
| |
Increase enalapril to 40mg orally daily
| |
Add digoxin 0.25mg orally daily
| |
Change carvedilol 3.25mg to metoprolol tartrate 25mg orally twice daily |
Question 70 Explanation:
The next appropriate course of action would be to increase Carvedilol. Since all diuretics have been stopped and her hemodynamics stable, initiating a beta-blocker is appropriate. The dose would be gradually increased every 2 weeks to the highest dose tolerable. She would also be monitored for congestive signs and symptoms of HF
Digoxin would not be added. Even though digoxin can improve symptoms in mild to moderate HF, long-term treatment had no effect on mortality. It does have the potential to decrease hospitalizations for HF. Carvedilol would not be changed to metoprolol tartrate since metoprolol tartrate was found to be less effective in patients with heart failure. Enalapril would not be increased.
Reference
Yancy CW, Jessup M, Bozkurt B, et al. 2013 ACCF/AHA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines.J Am Coll Cardiol. 2013;62(16):e147-e239. doi:10.1016/j.jacc.2013.05.019. Retirved on Feb 6th from : http://circ.ahajournals.org/content/128/16/e240
Reference
Yancy CW, Jessup M, Bozkurt B, et al. 2013 ACCF/AHA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines.J Am Coll Cardiol. 2013;62(16):e147-e239. doi:10.1016/j.jacc.2013.05.019. Retirved on Feb 6th from : http://circ.ahajournals.org/content/128/16/e240
Question 71 |
Proportion of people in a population who have a particular disease at a specified point in time or over a specified period of time is defined as which of the following?
Incidence rate
| |
Prevalence rate
| |
Mortality rate
| |
Relative risk |
Question 71 Explanation:
Incidence rate = New reported cases / summed person-years of observation (avg population during time interval)
Prevalence = Cases in a population in a given time period / total population at that time
I. Dicker, R. C., Coronado, F., Koo, D., et al. Principals of Epidemiology in Public Health Practice, Third Edition: An Introduction to Applied Epidemiology and Biostatistics; Lesson 3, Section 2. Oct. 2006 Retrieved Jan. 24, 2017 from: https://www.cdc.gov/ophss/csels/dsepd/ss1978/lesson3/section2.html Updated: Nov. 2011 II. Numerators, denominators and populations at risk. Jun. 20, 2010. Retrieved Jan. 24, 2017 from: http://www.healthknowledge.org.uk/public-health-textbook/research-methods/1a-epidemiology/numerators-denominators-populations
I. Dicker, R. C., Coronado, F., Koo, D., et al. Principals of Epidemiology in Public Health Practice, Third Edition: An Introduction to Applied Epidemiology and Biostatistics; Lesson 3, Section 2. Oct. 2006 Retrieved Jan. 24, 2017 from: https://www.cdc.gov/ophss/csels/dsepd/ss1978/lesson3/section2.html Updated: Nov. 2011 II. Numerators, denominators and populations at risk. Jun. 20, 2010. Retrieved Jan. 24, 2017 from: http://www.healthknowledge.org.uk/public-health-textbook/research-methods/1a-epidemiology/numerators-denominators-populations
Question 72 |
PG is a 86 YOW, weight 182 pounds, height 5’10”. Past medical history of hypertension, GI bleed, osteoarthritis, renal failure stage 4 (GFR = 15-30 mL/min), CHF with preserved ejection fraction. Her BP is 142/ 92, A1c 9.3. Her current medications are metformin 500mg by mouth BID, insulin glargine 20 units SQ at bedtime, atorvastatin 20mg by mouth daily, lisinopril 5mg by mouth daily, diltiazem 360mg daily, pantoprazole 40mg BID, acetaminophen 650mg q6hr. Which of the following would be the most appropriate option for management of his type 2 diabetes Mellitus?
Discontinue metformin and pioglitazone 30mg by mouth daily
| |
Discontinue metformin add empagliflozin 10mg by mouth daily | |
Discontinue metformin add empagliflozin 10mg by mouth daily and exenatide 2mg SQ once weekly
| |
Discontinue metformin and increase insulin glargine 30 units and add 5 units lispro subcutaneously TID |
Question 72 Explanation:
Pioglitazone is not a good option since it can exacerbate his CHF and caries a black box warning. Empagliflozin is not a good option since it is contraindicated in patients with eGFR <30. Exenatide use is not recommended in patients with CrCL<30 mls/hr. Exenatide is not a good option because the patient’s hx of GI bleed is a precaution for use since the drug can slow gastric emptying. Increasing patient’s long acting insulin and adding low dose short acting is an appropriate choice.
Reference:
I. American Diabetes Association. In Standards of Medical Care in Diabetes 2016. Diabetes Care 2016;39(Suppl. 1) Avaiable at: http://care.diabetesjournals.org/content/suppl/2015/12/21/39.Supplement_1.DC2/2016-Standards-of-Care.pdf II. Garber AJ, et al. Consensus Statement by the American Association of Clinical Endocrinologists and American College of Endocrinology on the Comprehensive Type 2 Diabetes Management Algorithm – 2016 Executive Summary. Endocr Pract. 2016; 22(1):84-113. Retrieved on Feb 8th, 2017 from : http://journals.aace.com/doi/10.4158/EP151126.CS
Reference:
I. American Diabetes Association. In Standards of Medical Care in Diabetes 2016. Diabetes Care 2016;39(Suppl. 1) Avaiable at: http://care.diabetesjournals.org/content/suppl/2015/12/21/39.Supplement_1.DC2/2016-Standards-of-Care.pdf II. Garber AJ, et al. Consensus Statement by the American Association of Clinical Endocrinologists and American College of Endocrinology on the Comprehensive Type 2 Diabetes Management Algorithm – 2016 Executive Summary. Endocr Pract. 2016; 22(1):84-113. Retrieved on Feb 8th, 2017 from : http://journals.aace.com/doi/10.4158/EP151126.CS
Question 73 |
PG is a 86 YOW, weight 182 pounds, height 5’10”. Past medical history of hypertension, GI bleed, osteoarthritis, renal failure stage 4 (GFR = 15-30 mL/min), CHF with preserved ejection fraction. Her BP is 142/ 92, A1c 9.3. Her current Metformin 500mg by mouth BID, Insulin glargine 20 units SQ at bedtime, Atorvastatin 20mg by mouth daily, Lisinopril 5mg by mouth daily, Diltiazem 360mg daily, pantoprazole 40mg BID, Acetaminophen 650mg q6hr. What should be PG’s goal A1c?
<6.5
| |
<7.5
| |
<8.0
| |
<8.5 |
Question 73 Explanation:
The patients A1C goal should be <8 because they have multiple chronic illnesses of HTN, CKD stage 4, osteoarthritis, and heart failure and they are elderly. The patient does not have end stage chronic illness that meets the <8.5 criteria. The <7.5% goal is solely due to age >65 years. The <7% goal is for non, elderly, healthy adults per ADA. The goal <6.5 is only for healthy, non elderly adults per AACE/ACE.
Reference:
I. American Diabetes Association. In Standards of Medical Care in Diabetes 2016. Diabetes Care 2016;39(Suppl. 1) Avaiable at: http://care.diabetesjournals.org/content/suppl/2015/12/21/39.Supplement_1.DC2/2016-Standards-of-Care.pdf II. Garber AJ, et al. Consensus Statement by the American Association of Clinical Endocrinologists and American College of Endocrinology on the Comprehensive Type 2 Diabetes Management Algorithm – 2016 Executive Summary. Endocr Pract. 2016; 22(1):84-113. Retrieved on Feb 8th, 2017 from : http://journals.aace.com/doi/10.4158/EP151126.CS
Reference:
I. American Diabetes Association. In Standards of Medical Care in Diabetes 2016. Diabetes Care 2016;39(Suppl. 1) Avaiable at: http://care.diabetesjournals.org/content/suppl/2015/12/21/39.Supplement_1.DC2/2016-Standards-of-Care.pdf II. Garber AJ, et al. Consensus Statement by the American Association of Clinical Endocrinologists and American College of Endocrinology on the Comprehensive Type 2 Diabetes Management Algorithm – 2016 Executive Summary. Endocr Pract. 2016; 22(1):84-113. Retrieved on Feb 8th, 2017 from : http://journals.aace.com/doi/10.4158/EP151126.CS
Question 74 |
In a cohort study of 47,363 male US health professionals, the Health Professionals Follow-up Study (HPFS), regular aspirin use (≥2 times/week) found (RR, 0.79; 95% CI, 0.69–0.90) for colorectal cancer over 18 years of follow-up. How can this data best be interpreted?
I. Those who take aspirin ≥2 times/week have 0.79 times the risk of colorectal cancer
II. Those who take aspirin ≥2 times/week have 0.21 times the risk of colorectal cancer
III. Those who take aspirin ≥2 times/week have 21% lower risk of colorectal cancer
IV. Those who take aspirin ≥2 times/week have 79% lower risk of colorectal cancer
II
| |
II and III
| |
I and IV
| |
I and III
|
Question 74 Explanation:
Relative risk can be stated as 0.79 times as likely or 0.79 times the risk, but it could also be illustrated as a relative risk reduction and stated as a 21% risk reduction or 21% lower risk by taking the medication.
Reference:
I. Irwig, Les. Chapter 18: Relative risk, relative and absolute risk reduction, number needed to treat and confidence intervals. Smart health choices: making sense of health advice. Judy Irwig, 2007. Retrieved Jan. 24, 2017 from: https://www.ncbi.nlm.nih.gov/books/NBK63647/ II. Confidence Intervals for the Risk Ratio (Relative Risk). (n.d.) Retrieved Jan. 24, 2017 from: http://sphweb.bumc.bu.edu/otlt/mph-modules/bs/bs704_confidence_intervals/bs704_confidence_intervals8.html
Reference:
I. Irwig, Les. Chapter 18: Relative risk, relative and absolute risk reduction, number needed to treat and confidence intervals. Smart health choices: making sense of health advice. Judy Irwig, 2007. Retrieved Jan. 24, 2017 from: https://www.ncbi.nlm.nih.gov/books/NBK63647/ II. Confidence Intervals for the Risk Ratio (Relative Risk). (n.d.) Retrieved Jan. 24, 2017 from: http://sphweb.bumc.bu.edu/otlt/mph-modules/bs/bs704_confidence_intervals/bs704_confidence_intervals8.html
Question 75 |
WM did not receive influenza vaccine prior to the start of this season, it’s now December. He did get influenza vaccine last year. Which of the following is correct course of action?
Skip influenza vaccine for this year since it’s too late.
| |
Skip influenza vaccine for this year since he received vaccine last year.
| |
Start WM on Tamiflu to prevent him from getting influenza.
| |
Vaccinate him with influenza vaccine since influenza season lasts until March in your community. |
Question 75 Explanation:
Influenza vaccine is recommended annually, thus, WM should not skip it this year, and B is incorrect. Also, per the CDC, seasonal influenza outbreaks can occur as early as October, however, most activity peaks in January or later. Thus, it is not too late for WM to receive his vaccine in December, thus A is incorrect. Lastly, antiviral medications such as Tamiflu are an important adjunct to vaccinations. They are recommended as early as possible for any patient with confirmed or suspected influenza who, is 1) Hospitalized, 2) has severe, complicated, or progressive illness or 3) is at higher risk for influenza complications. Thus, WM is not a candidate with the given information and C is incorrect.
Reference:
Key Facts About Seasonal Flu Vaccine. Centers for Disease Control and Prevention. 2016. Available at: http://www.cdc.gov/flu/protect/keyfacts.htm. Accessed September 27, 2016.
Reference:
Key Facts About Seasonal Flu Vaccine. Centers for Disease Control and Prevention. 2016. Available at: http://www.cdc.gov/flu/protect/keyfacts.htm. Accessed September 27, 2016.
Question 76 |
In the US Nurses’ Health Study (NHS) cohort study, where they looked at association of regular aspirin use (≥two 325 mg tablets/week) and colorectal cancer in 82,911 women found (RR, 0.77; 95% CI, 0.67–0.88) over 20 years of follow-up. In another analysis of the NHS, regular aspirin use, investigator also found (hazard ratio [HR]=0.72, 95% CI 0.56–0.92), what does this say about the mortality from colorectal cancer?
How can this data best be interpreted?
Those who take aspirin ≥2 times/week have 23% lower risk of colorectal cancer
| |
Those who take aspirin ≥2 times/week have 0.77% lower risk of colorectal cancer
| |
Those who take aspirin ≥2 times/week have 28% lower risk of colorectal cancer
| |
Those who take aspirin ≥2 times/week have 23% reduction in death from colorectal cancer |
Question 76 Explanation:
. Relative risk can be stated as 0.77 times as likely or 0.77 times the risk, but it could also be illustrated as a relative risk reduction and stated as a 23% risk reduction or 23% lower risk by taking the medication.
Reference:
Irwig, Les. Chapter 18: Relative risk, relative and absolute risk reduction, number needed to treat and confidence intervals. Smart health choices: making sense of health advice. Judy Irwig, 2007. Retrieved Jan. 24, 2017 from: https://www.ncbi.nlm.nih.gov/books/NBK63647/
Reference:
Irwig, Les. Chapter 18: Relative risk, relative and absolute risk reduction, number needed to treat and confidence intervals. Smart health choices: making sense of health advice. Judy Irwig, 2007. Retrieved Jan. 24, 2017 from: https://www.ncbi.nlm.nih.gov/books/NBK63647/
Question 77 |
In the US Nurses’ Health Study (NHS) cohort study, where they looked at association of regular aspirin use (≥two 325 mg tablets/week) and colorectal cancer in 82,911 women found (RR, 0.77; 95% CI, 0.67–0.88) over 20 years of follow-up. In an another analysis of the NHS, regular aspirin use, investigator also found (hazard ratio [HR]=0.72, 95% CI 0.56–0.92), what does this say about the mortality from colorectal cancer? How can this data best be interpreted?
Those who takes aspirin regularly have 72% lower risk of colorectal cancer
| |
Those who takes aspirin regularly have 28% reduction in death from colorectal cancer
| |
Those who takes aspirin regularly have 0.23% lower risk of colorectal cancer
| |
Those who takes aspirin regularly have 77% lower risk of colorectal cancer |
Question 77 Explanation:
Hazard ratio can be used to compare time-to-event data between 2 groups. In this case the time to event was 20 years-to-death from colorectal cancer and the groups were patients taking aspirin 325mg 2 or more times a week and patients that did not. With the HR being 0.72, the patients taking the aspirin were 0.72 times likely to die at any time during the 20 years. This means that aspirin had a 28% reduction in death from colorectal cancer, 1 – 0.72 = 0.28.
Reference:
Sedgwick, Philip, and Katherine Joekes. "Interpreting hazard ratios." BMJ: British Medical Journal 351 (2015).
Reference:
Sedgwick, Philip, and Katherine Joekes. "Interpreting hazard ratios." BMJ: British Medical Journal 351 (2015).
Question 78 |
JM is a 72 YOM who comes to the ER with gastroenteritis. After reviewing his vaccination records you find that he has received 1 dose of Tdap when he was 60 years old, had influenza vaccine and PPSV23 3 years ago when he was admitted in the hospital for exacerbation of HF. It is Oct 2016, what vaccine should JM receive?
Influenza
| |
PCV13 and Influenza
| |
Influenza, PCV13, Zoster and Td booster
| |
Influenza, PCV13, Zoster, Td booster and MMR |
Question 78 Explanation:
Influenza vaccine is recommended annually, thus JM is a candidate, as he hasn’t received it since 2013. Patient is also a candidate for the herpes zoster vaccine as he is over the age of 60. A Tdap booster is recommended every 10 years, thus JM is a candidate as his last Tdap was 12 years ago. Lastly, patient is a candidate for the PCV13 vaccine as it is recommend 1 or more years after PPSV23 shot (given 3 yeas ago.) Patient is not a candidate for MMR, as individuals, who have been born prior to 1957 are considered immune to measles and mumps (patient born in 1944.)
Reference:
Adult Immunization Schedule. Centers for Disease Control and Prevention. http://www.cdc.gov/vaccines/schedules/hcp/adult.html. Updated April 20, 2016. Accessed September 5, 2016
Reference:
Adult Immunization Schedule. Centers for Disease Control and Prevention. http://www.cdc.gov/vaccines/schedules/hcp/adult.html. Updated April 20, 2016. Accessed September 5, 2016
Question 79 |
Which of the following would be most appropriate to treat stenotrophomonas maltophilia?
Meropenem
| |
Vancomycin
| |
Ciprofloxacin
| |
Sulfamethoxazole/trimethoprim |
Question 79 Explanation:
Primary treatment for stenotrophomonas maltophilia is SMX-TMP. Meropenem, ciprofloxacin, and vancomycin have no coverage.
Reference:
Gilbert D. The Sanford Guide to Antimicrobial Therapy 2014. Sperryville, Va.: Antimicrobial Therapy; 2014
Reference:
Gilbert D. The Sanford Guide to Antimicrobial Therapy 2014. Sperryville, Va.: Antimicrobial Therapy; 2014
Question 80 |
The rate that an outcome will occur given a particular exposure, compared to the rate of the outcome occurring in the absence of that exposure is definition of which of the following?
Incidence rate
| |
Prevelance rate
| |
Odds ratio
| |
Relative risk |
Question 80 Explanation:
RR = rate of an outcome occurring in an exposed group (treatment group/intervention group) divided by the rate of an outcome occurring in an unexposed group (control group)
Ex: Relative Risk = Rate of UTI in patients taking drug XYZ / rate of UTI in patients not on drug XYZ
Reference:
I. 2x2 Contingency Table with Odds Ratios, etc. (n.d.). Retrieved Jan. 24, 2017 from: http://www.vassarstats.net/odds2x2.html II. Szumilas, M. "Explaining odds ratios." J Can Acad Child Adolesc Psychiatry 19 (2010): 227. Retrieved Jan. 24, 2017 from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2938757/
Reference:
I. 2x2 Contingency Table with Odds Ratios, etc. (n.d.). Retrieved Jan. 24, 2017 from: http://www.vassarstats.net/odds2x2.html II. Szumilas, M. "Explaining odds ratios." J Can Acad Child Adolesc Psychiatry 19 (2010): 227. Retrieved Jan. 24, 2017 from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2938757/
Question 81 |
JK is a 67 years African American man who presents to your clinic for his blood pressure management. His past medical history includes peptic ulcer disease and hypertension. His two BP readings are 160/98, 159/96 and HR 85. He says he has been adherent to his medications and lifestyle. He currently takes 12.5mg chlorthalidone and prilosec 20mg daily. Which of the following is the best strategy to manage his blood pressure?
Increase chlorthalidone to 25mg daily
| |
Add Norvasc 2.5 daily
| |
Add Lisinopril 5mg daily
| |
Strategies A or B could be used |
Question 81 Explanation:
As the patient is over the age of 60 and he does not have CKD or diabetes, his goal BP should be SBP < 150 mmHg or DBP < 90 mmHg, and he is not currently at this goal with his medication regimen. Options are to maximize the current medication dosage (option A), or to add a second agent. Since calcium channel blockers like Norvasc are recommended as initial treatment options in African Americans, choosing Norvasc over lisinopril would probably be the more effective option.
Reference:
James P, Oparil S, Carter B et al. 2014 Evidence-Based Guideline for the Management of High Blood Pressure in Adults. JAMA. 2014;311(5):507. doi:10.1001/jama.2013.284427. Retrieved Jan. 24, 2017 from: http://jamanetwork.com/journals/jama/fullarticle/1791497
Reference:
James P, Oparil S, Carter B et al. 2014 Evidence-Based Guideline for the Management of High Blood Pressure in Adults. JAMA. 2014;311(5):507. doi:10.1001/jama.2013.284427. Retrieved Jan. 24, 2017 from: http://jamanetwork.com/journals/jama/fullarticle/1791497
Question 82 |
Results from a Meta-analysis where they looked at frequency of postoperative atrial fibrillation in patients on ascorbic acid after cardiac surgery found odds ratio, 0.44 (95% CI, 0.32 to 0.61). How can you interpret this data?
Ascorbic acid increased frequency of postoperative arterial fibrillation after cardiac surgery by 44%
| |
Ascorbic acid decreased frequency of postoperative arterial fibrillation after cardiac surgery by 44%
| |
There was no statistically significant difference in frequency of postoperative arterial fibrillation after cardiac surgery
| |
Ascorbic acid decreased frequency of postoperative arterial fibrillation after cardiac surgery by 56% |
Question 82 Explanation:
Odds ratio of 0.44 (44%) means that this group was associated with an event happening 44% of the time, compared to 1 (an event happening 100% of the time if unexposed), therefore 100 - 44 = 56%, which is the reduction caused by the exposure. Exposure is the use of ascorbic acid.
Reference:
Davies, Huw Talfryn Oakley, Iain Kinloch Crombie, and Manouche Tavakoli. "When can odds ratios mislead?." Bmj 316.7136 (1998): 989-991. Retrieved Jan. 24, 2017 from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1112884/
Reference:
Davies, Huw Talfryn Oakley, Iain Kinloch Crombie, and Manouche Tavakoli. "When can odds ratios mislead?." Bmj 316.7136 (1998): 989-991. Retrieved Jan. 24, 2017 from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1112884/
Question 83 |
The Management of Adults with Hospital-acquired and Ventilator-associated Pneumonia: 2016 Clinical Practice Guidelines by the Infectious Diseases Society of America and the American Thoracic Society recommends covering what bacteria empirically for suspected VAP?
S. aureus and Pseudomonas aeruginosa
| |
Streptococcus and Pseudomonas aeruginosa
| |
Pseudomonas aeruginosa and ESBL
| |
S. aureus plus Streptococcus |
Question 83 Explanation:
These bacteria are some of the ones most commonly associated with VAP in the United States. This is based on surveillance data. They are also some of the most frequent isolates identified in international surveillance programs. Therefore, the guidelines recommend treatment to cover these bacteria.
Reference:
Kalil AC, Metersky ML, Klompas M, et al. Management of Adults With Hospital-acquired and Ventilator-associated Pneumonia: 2016 Clinical Practice Guidelines by the Infectious Diseases Society of America and the American Thoracic Society. Clin Infect Dis. 2016;ciw353. doi:10.1093/cid/ciw353. Retrieved on feb 8th, 2017 from : https://academic.oup.com/cid/article/63/5/e61/2237650/Management-of-Adults-With-Hospital-acquired-and
Reference:
Kalil AC, Metersky ML, Klompas M, et al. Management of Adults With Hospital-acquired and Ventilator-associated Pneumonia: 2016 Clinical Practice Guidelines by the Infectious Diseases Society of America and the American Thoracic Society. Clin Infect Dis. 2016;ciw353. doi:10.1093/cid/ciw353. Retrieved on feb 8th, 2017 from : https://academic.oup.com/cid/article/63/5/e61/2237650/Management-of-Adults-With-Hospital-acquired-and
Question 84 |
Which of the following sulfonylureas is listed as a potentially inappropriate medication in elderly according to AGS updated beers criteria?
Glyburide
| |
Glipizide
| |
Glimepiride
| |
A and B |
Question 84 Explanation:
In Table 2, the AGS states that glyburide is risky because of the possibility of severe prolonged hypoglycemia. Also mentioned in this section is Chlorpropamide, which has a prolonged half-life in older adults and can cause SIADH or prolonged hypoglycemia.
Reference:
Radcliff, Sue, et al. "American Geriatrics Society 2015 updated beers criteria for potentially inappropriate medication use in older adults." JOURNAL OF THE AMERICAN GERIATRICS SOCIETY 63.11 (2015): 2227-2246. Available at: http://onlinelibrary.wiley.com/doi/10.1111/jgs.13702/full
Reference:
Radcliff, Sue, et al. "American Geriatrics Society 2015 updated beers criteria for potentially inappropriate medication use in older adults." JOURNAL OF THE AMERICAN GERIATRICS SOCIETY 63.11 (2015): 2227-2246. Available at: http://onlinelibrary.wiley.com/doi/10.1111/jgs.13702/full
Question 85 |
Number of new cases per population at risk in a given time period is a definition of which of the following?
Incidence rate
| |
Prevalence rate
| |
Mortality rate
| |
Odds ratio |
Question 85 Explanation:
Incidence rate = New reported cases / summed person-years of observation (avg population during time interval). Prevalence = Cases in a population in a given time period / total population at that time Mortality rate = deaths during specified time interval / population size at risk for death
Reference:
Dicker, R. C., Coronado, F., Koo, D., et al. Principals of Epidemiology in Public Health Practice, Third Edition: An Introduction to Applied Epidemiology and Biostatistics; Lesson 3, Section 2. Oct. 2006 Retrieved Jan. 24, 2017 from: https://www.cdc.gov/ophss/csels/dsepd/ss1978/lesson3/section2.html Updated: Nov. 2011
Reference:
Dicker, R. C., Coronado, F., Koo, D., et al. Principals of Epidemiology in Public Health Practice, Third Edition: An Introduction to Applied Epidemiology and Biostatistics; Lesson 3, Section 2. Oct. 2006 Retrieved Jan. 24, 2017 from: https://www.cdc.gov/ophss/csels/dsepd/ss1978/lesson3/section2.html Updated: Nov. 2011
Question 86 |
Which of the following gastroenterological changes is/are seen as the body ages?
Decrease in gastric pH
| |
Decrease in gastric blood flow
| |
Increased gastric emptying
| |
A and B |
Question 86 Explanation:
Aging has been associated with various GI changes such as: a decrease in splanchnic blood flow, delayed gastric emptying, and an increase in gastric pH.
Reference:
Mangoni AJackson S. Age-related changes in pharmacokinetics and pharmacodynamics: basic principles and practical applications. British Journal of Clinical Pharmacology. 2003;57(1):6-14. doi:10.1046/j.1365-2125.2003.02007.x.
Reference:
Mangoni AJackson S. Age-related changes in pharmacokinetics and pharmacodynamics: basic principles and practical applications. British Journal of Clinical Pharmacology. 2003;57(1):6-14. doi:10.1046/j.1365-2125.2003.02007.x.
Question 87 |
Which of the following diagnostic lab test is recommended by the Management of Adults With Hospital-acquired and Ventilator-associated Pneumonia: 2016 Clinical Practice Guidelines by the Infectious Diseases Society of America and the American Thoracic Society in addition to clinical criteria to guide discontinuation of antibiotics?
Procalcitonin (PCT)
| |
C - Reactive protein (CRP)
| |
Modified Clinical Pulmonary Infection Score (CPIS)
| |
Clinical Criteria alone |
Question 87 Explanation:
The use of PCT levels can decrease antibiotic exposure without increasing treatment failure or mortality. As a result, costs are reduced as well as the occurrence of side effects. Current evidence does not support the use of CPIS to guide discontinuation of antibiotics since it is not reliable enough to determine whether antibiotic therapy should be continued or not. CRP was not mentioned in the guidelines as to whether it can be used to determine discontinuation of antibiotic therapy or not.
Reference:
Kalil AC, Metersky ML, Klompas M, et al. Management of Adults With Hospital-acquired and Ventilator-associated Pneumonia: 2016 Clinical Practice Guidelines by the Infectious Diseases Society of America and the American Thoracic Society. Clin Infect Dis. 2016;ciw353. doi:10.1093/cid/ciw353. Retrieved on feb 8th, 2017 from : https://academic.oup.com/cid/article/63/5/e61/2237650/Management-of-Adults-With-Hospital-acquired-and
Reference:
Kalil AC, Metersky ML, Klompas M, et al. Management of Adults With Hospital-acquired and Ventilator-associated Pneumonia: 2016 Clinical Practice Guidelines by the Infectious Diseases Society of America and the American Thoracic Society. Clin Infect Dis. 2016;ciw353. doi:10.1093/cid/ciw353. Retrieved on feb 8th, 2017 from : https://academic.oup.com/cid/article/63/5/e61/2237650/Management-of-Adults-With-Hospital-acquired-and
Question 88 |
CJ is a 69 year old male with a history of diabetes, hypertension and hypercholesterolemia. His fasting lipid profile is TC 530 mg/dL; LDL-C 125; HDL-C 48 mg/dL; and TG 640 mg/dL. His A1c 8.1, calculate creatinine clearance is 65mls/hr, BP 135/80 mm Hg, HR 70 beats /min. His current medications includes metformin 1000mg po bid, lisinopril 20mg daily, sitagliptin 50mg bid and atorvastatin 40mg daily. What is the best pharmacological agent to initiate on CJ?
Increase atorvastatin to 80mg
| |
Niacin 500mg twice daily
| |
Fenofibrate 162mg daily
| |
Gemfibrozil 600mg twice daily |
Question 88 Explanation:
It is reasonable to add triglyceride-lowering medications such as fibrates or niacin to prevent pancreatitis in those with triglyceride levels >500 mg/dL, which applies to this patient as his TG level is 640 mg/dL . C. is wrong because gemfibrozil should not be initiated in patients on statin therapy because of an increased risk for muscle symptoms and rhabdomyolysis. Fenofibrate may be considered concomitantly with a low- or moderate- intensity statin when triglycerides are above 500 mg/dL,2, however he is on a high intensity statin therapy. For niacin, the IR dose should start at 100 mg TID2 and niacin does not lower triglyceride levels as much as fibrate do.4 Fenofibrates are dose adjusted for renal function lower than 60 mL/min to 54 mg/mL, so this dose is appropriate for this patient because of his renal function being above 60 mL/min. The best option is fenofibrate 162 mg daily, but this needs to be monitored for any symptoms of muscle pain exhibited by the patient, especially as the patient is at a higher risk due to being a diabetic.
Reference:
I. Stone N, Robinson J, Lichtenstein A et al. 2013 ACC/AHA Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults. Circulation. 2013;129(25 suppl 2):S1-S45. doi:10.1161/01.cir.0000437738.63853.7a. Retrieved on Feb 6th 2017 from : http://circ.ahajournals.org/content/129/25_suppl_2/S1
II. Miller M, Stone N, Ballantyne C et al. Triglycerides and Cardiovascular Disease: A Scientific Statement From the American Heart Association. Circulation. 2011;123(20):2292-2333. doi:10.1161/cir.0b013e3182160726.
Reference:
I. Stone N, Robinson J, Lichtenstein A et al. 2013 ACC/AHA Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults. Circulation. 2013;129(25 suppl 2):S1-S45. doi:10.1161/01.cir.0000437738.63853.7a. Retrieved on Feb 6th 2017 from : http://circ.ahajournals.org/content/129/25_suppl_2/S1
II. Miller M, Stone N, Ballantyne C et al. Triglycerides and Cardiovascular Disease: A Scientific Statement From the American Heart Association. Circulation. 2011;123(20):2292-2333. doi:10.1161/cir.0b013e3182160726.
Question 89 |
SJ is a 71 YOM, weight 253 pounds, height 5’ 11”. Past medical history gout, hypertension, dyslipidemia, COPD and pancreatitis while on Sitagliptin. His BP is 138/88, A1c is 9.4. Serum creatinine 1.0mg/dL. His current medications includes, Metformin 1000mg BID, Insulin glargine 30 units SQ at bedtime, Acarbose 100mg tid, Atorvastatin 80mg by mouth daily, Ramipril 10mg by mouth daily, Tiotropium 18mcg inhaled daily. Which of the following would be the most appropriate option for management of his type 2 diabetes Mellitus?
Add Empagliflozin 10mg by mouth daily
| |
Add Exenatide 2mg SQ once weekly
| |
Add Linagliptin 5mg by mouth daily
| |
Increase Insulin glargine 60 units and add Insulin Lispro sliding scale |
Question 89 Explanation:
Empagliflozin is the best option for this patient. Linagliptin is not an option since patient has already tried Sitagliptin (in the same drug class), and patient had pancreatitis. GLP1- agonists also are associated with pancreatitis so use of Exenatide would not be recommended. Pioglitazone should not be used because the patient is ~52% overweight and it can cause weight gain. Increasing the long acting insulin dose and adding short acting sliding scale is an not an appropriate option since sliding scale in elderly adults in on the BEERs list due to potential increased risk of errors/hypoglycemia.
Reference:
I. American Diabetes Association. In Standards of Medical Care in Diabetes 2016. Diabetes Care 2016;39(Suppl. 1) Avaiable at: http://care.diabetesjournals.org/content/suppl/2015/12/21/39.Supplement_1.DC2/2016-Standards-of-Care.pdf
II. Food and Drug Administration (US FDA) Drug Medwatch-FDA investigating reports of possible increased risk of pancreatitis and pre-cancerous findings of the pancreas from incretin mimetic drugs for type 2 diabetes. Retrieved Mar. 14, 2013. Available on the World Wide Web at http://www.fda.gov/Drugs/DrugSafety/ucm343187.htm.
III. Radcliff, Sue, et al. "American Geriatrics Society 2015 updated beers criteria for potentially inappropriate medication use in older adults." JOURNAL OF THE AMERICAN GERIATRICS SOCIETY 63.11 (2015): 2227-2246. Available at: http://onlinelibrary.wiley.com/doi/10.1111/jgs.13702/full
Reference:
I. American Diabetes Association. In Standards of Medical Care in Diabetes 2016. Diabetes Care 2016;39(Suppl. 1) Avaiable at: http://care.diabetesjournals.org/content/suppl/2015/12/21/39.Supplement_1.DC2/2016-Standards-of-Care.pdf
II. Food and Drug Administration (US FDA) Drug Medwatch-FDA investigating reports of possible increased risk of pancreatitis and pre-cancerous findings of the pancreas from incretin mimetic drugs for type 2 diabetes. Retrieved Mar. 14, 2013. Available on the World Wide Web at http://www.fda.gov/Drugs/DrugSafety/ucm343187.htm.
III. Radcliff, Sue, et al. "American Geriatrics Society 2015 updated beers criteria for potentially inappropriate medication use in older adults." JOURNAL OF THE AMERICAN GERIATRICS SOCIETY 63.11 (2015): 2227-2246. Available at: http://onlinelibrary.wiley.com/doi/10.1111/jgs.13702/full
Question 90 |
What is the recommendation according to the AGS Updated beers Criteria when using SNRIs, SSRIs and TCAs in older adults?
Avoid use, it may exacerbate or cause syndrome of inappropriate antidiuretic hormone secretion or hyponatremia
| |
Use with caution, it may exacerbate or may cause syndrome of inappropriate antidiuretic hormone secretion or hyponatremia
| |
Use with caution in adult aged ≥75 years, it may exacerbate or may cause syndrome of inappropriate antidiuretic hormone secretion or hyponatremia
| |
Use with caution is patients with creatinine clearance < 30 mls/hr, it may exacerbate or may cause syndrome of inappropriate antidiuretic hormone secretion or hyponatremia |
Question 90 Explanation:
In Table 4, the AGS recommends to use these medications with caution, the patient should be monitored for these conditions. Other medications that have the potential to cause SIADH or hyponatremia include: Antipsychotics, Diuretics, Carbamazepine, Oxcarbazepine, Carboplatin, Cisplatin, Vincristine, and Mirtazapine.
Reference:
Radcliff, Sue, et al. "American Geriatrics Society 2015 updated beers criteria for potentially inappropriate medication use in older adults." JOURNAL OF THE AMERICAN GERIATRICS SOCIETY 63.11 (2015): 2227-2246. Available at: http://onlinelibrary.wiley.com/doi/10.1111/jgs.13702/full
Reference:
Radcliff, Sue, et al. "American Geriatrics Society 2015 updated beers criteria for potentially inappropriate medication use in older adults." JOURNAL OF THE AMERICAN GERIATRICS SOCIETY 63.11 (2015): 2227-2246. Available at: http://onlinelibrary.wiley.com/doi/10.1111/jgs.13702/full
Question 91 |
If 70 % of S. aureus isolated in your ICU are methicillin resistance, what anti-staphylococcus antibiotic should you use to treat suspected VAP?
piperacillin-tazobactam
| |
Oxacillin
| |
Vancomycin
| |
Moxifloxacin |
Question 91 Explanation:
Since there is 70% of S. aureus isolate in the ICU that is methicillin resistant, vancomycin would be indicated since it is the only agent of the options given above that has activity against MRSA.
Reference:
Kalil AC, Metersky ML, Klompas M, et al. Management of Adults With Hospital-acquired and Ventilator-associated Pneumonia: 2016 Clinical Practice Guidelines by the Infectious Diseases Society of America and the American Thoracic Society. Clin Infect Dis. 2016;ciw353. doi:10.1093/cid/ciw353. Retrieved on feb 8th, 2017 from : https://academic.oup.com/cid/article/63/5/e61/2237650/Management-of-Adults-With-Hospital-acquired-and
Reference:
Kalil AC, Metersky ML, Klompas M, et al. Management of Adults With Hospital-acquired and Ventilator-associated Pneumonia: 2016 Clinical Practice Guidelines by the Infectious Diseases Society of America and the American Thoracic Society. Clin Infect Dis. 2016;ciw353. doi:10.1093/cid/ciw353. Retrieved on feb 8th, 2017 from : https://academic.oup.com/cid/article/63/5/e61/2237650/Management-of-Adults-With-Hospital-acquired-and
Question 92 |
All of the following may increase triglycerides except?
Protease inhibitor
| |
Bile acid sequestrants
| |
Fish Oil
| |
Oral estrogens |
Question 92 Explanation:
Agents that can cause elevated triglycerides: oral estrogens, glucocorticoids, bile acid sequestrants, protease inhibitors, retinoic acid, anabolic steroids, sirolimus, raloxifene, tamoxifen, beta blockers (not carvedilol), and thiazides.
Reference:
Stone N, Robinson J, Lichtenstein A et al. 2013 ACC/AHA Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults. Circulation. 2013;129(25 suppl 2):S1-S45. doi:10.1161/01.cir.0000437738.63853.7a. Retrieved on Feb 6th 2017 from : http://circ.ahajournals.org/content/129/25_suppl_2/S1
Reference:
Stone N, Robinson J, Lichtenstein A et al. 2013 ACC/AHA Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults. Circulation. 2013;129(25 suppl 2):S1-S45. doi:10.1161/01.cir.0000437738.63853.7a. Retrieved on Feb 6th 2017 from : http://circ.ahajournals.org/content/129/25_suppl_2/S1
Question 93 |
SR is a 69 YOM, weight 236 pounds, height 5’8”. Past medical history includes hypertension, diabetes mellitus, CHF with reduced ejection fraction. His BP 137/86, A1c 9.7, Serum creatinine 1.0 mg/dL. His current medications include Metformin 1000mg by mouth BID, Insulin glargine 20 units SQ at bedtime, Glipizide 10mg by mouth twice daily. Atorvastatin 40mg by mouth daily, Lisinopril 20mg by mouth daily, Carvedilol 12.5mg BID, Furosemide 20mg by mouth daily and Spironolactone 12.5mg by mouth daily. SR also complains of several hypoglycemic episodes on days he skips meal or eats late.
Which of the following would be the most appropriate option for management of his type 2 diabetes Mellitus?
D/C Glipizide and add Pioglitazone 30mg by mouth daily
| |
D/C Glipizide and add Dapagliflozin 10mg by mouth daily
| |
D/C Glipizide and add Dulaglutide 0.75mg SQ once weekly
| |
Increase Insulin glargine 40 units and add Insulin Lispro sliding scale |
Question 93 Explanation:
Glipizide should be discontinued because it works by increasing insulin secretion and one of its main side effects is hypoglycemia. Since the patient does not eat stable meals, this is what is contributing to his episodes of hypoglycemia and this drug should not be used for him. Dapagliflozin would not get to goal A1c. Its A1c reduction capabilities is from 0.5% - 1%. Pioglitazone is not a good option for this patient since there is a black box warning for exacerbating heart failure. Dapagliflozin is not a good option since it works by reducing reabsorption in the kidney which can cause volume depletion in this patient who is already on furosemide. Adding Dulaglutide 0.75mg once weekly would simplify regimen and drop A1c to goal. GLP-1 agonist can drop A1c by average 1%-1.5%. Option D is not ideal either because increasing a long acting insulin glargine in addition to sliding scale will just contribute to hypoglycemia. Sliding scale insulin are potentially inappropriate medication per the beer’s criteria. IBW = 68.4 kg; actual BW = 107.3 kg. >120% overweight; adjBW = 84 kg, CrCL = 82.8 mL/min
Reference:
I. American Diabetes Association. In Standards of Medical Care in Diabetes 2016. Diabetes Care 2016;39(Suppl. 1) Avaiable at: http://care.diabetesjournals.org/content/suppl/2015/12/21/39.Supplement_1.DC2/2016-Standards-of-Care.pdf
II. Garber AJ, et al. Consensus Statement by the American Association of Clinical Endocrinologists and American College of Endocrinology on the Comprehensive Type 2 Diabetes Management Algorithm – 2016 Executive Summary. Endocr Pract. 2016; 22(1):84-113. Retrieved on Feb 8th, 2017 from : http://journals.aace.com/doi/10.4158/EP151126.CS
III. American Geriatrics Society 2015 Updated Beers Criteria for Potentially Inappropriate Medication Use in Older Adults. Journal of the American Geriatrics Society. 2015;63(11):2227-2246. doi:10.1111/jgs.13702.
IV. Actos (pioglitazone) package insert. Deerfield, IL: Takeda Pharmaceuticals America, Inc.; 2013 Nov.
V. Farxiga (dapagliflozin) package insert. Princeton, NJ: Bristol-Myers Squibb Company; 2016 Aug.
VI. Trulicity (dulaglutide) package insert. Indianapolis, IN: Eli Lilly and Company; 2014 Sept.
Reference:
I. American Diabetes Association. In Standards of Medical Care in Diabetes 2016. Diabetes Care 2016;39(Suppl. 1) Avaiable at: http://care.diabetesjournals.org/content/suppl/2015/12/21/39.Supplement_1.DC2/2016-Standards-of-Care.pdf
II. Garber AJ, et al. Consensus Statement by the American Association of Clinical Endocrinologists and American College of Endocrinology on the Comprehensive Type 2 Diabetes Management Algorithm – 2016 Executive Summary. Endocr Pract. 2016; 22(1):84-113. Retrieved on Feb 8th, 2017 from : http://journals.aace.com/doi/10.4158/EP151126.CS
III. American Geriatrics Society 2015 Updated Beers Criteria for Potentially Inappropriate Medication Use in Older Adults. Journal of the American Geriatrics Society. 2015;63(11):2227-2246. doi:10.1111/jgs.13702.
IV. Actos (pioglitazone) package insert. Deerfield, IL: Takeda Pharmaceuticals America, Inc.; 2013 Nov.
V. Farxiga (dapagliflozin) package insert. Princeton, NJ: Bristol-Myers Squibb Company; 2016 Aug.
VI. Trulicity (dulaglutide) package insert. Indianapolis, IN: Eli Lilly and Company; 2014 Sept.
Question 94 |
What should be SR’s goal A1c?
<6.5
| |
<7.0
| |
<7.5 | |
<8.5 |
Question 94 Explanation:
This patient is elderly >65 years old which qualifies him for A1C goal <7.5%. While they do have certain co-morbidities/chronic illnesses of CHF, stage 2 CKD (CrCl 82.8 mL/min), and HTN, this patient does not meet at least 3 chronic illnesses that meet the criteria per the guidelines to have a less stringent A1C goal of <8. This list consists of “arthritis, cancer, congestive heart failure, depression, emphysema, falls, hypertension, incontinence, stage 3 or worse chronic kidney disease, myocardial infarction, and stroke”. This patient only meets 2 of these. In order to meet goal for <8.5 goal A1C, the patient must qualify with presence of one of the following: “single end-stage chronic illness, such as stage 3–4 congestive heart failure or oxygen-dependent lung disease, chronic kidney disease requiring dialysis, or uncontrolled metastatic cancer”. The goal <6.5 is only for healthy, nonelderly adults per AACE/ACE.
Reference:
I. American Diabetes Association. In Standards of Medical Care in Diabetes 2016. Diabetes Care 2016;39(Suppl. 1) Avaiable at: http://care.diabetesjournals.org/content/suppl/2015/12/21/39.Supplement_1.DC2/2016-Standards-of-Care.pdf
II. Garber AJ, et al. Consensus Statement by the American Association of Clinical Endocrinologists and American College of Endocrinology on the Comprehensive Type 2 Diabetes Management Algorithm – 2016 Executive Summary. Endocr Pract. 2016; 22(1):84-113. Retrieved on Feb 8th, 2017 from : http://journals.aace.com/doi/10.4158/EP151126.CS
Reference:
I. American Diabetes Association. In Standards of Medical Care in Diabetes 2016. Diabetes Care 2016;39(Suppl. 1) Avaiable at: http://care.diabetesjournals.org/content/suppl/2015/12/21/39.Supplement_1.DC2/2016-Standards-of-Care.pdf
II. Garber AJ, et al. Consensus Statement by the American Association of Clinical Endocrinologists and American College of Endocrinology on the Comprehensive Type 2 Diabetes Management Algorithm – 2016 Executive Summary. Endocr Pract. 2016; 22(1):84-113. Retrieved on Feb 8th, 2017 from : http://journals.aace.com/doi/10.4158/EP151126.CS
Question 95 |
Marked limitation of physical activity, comfortable at rest, but ordinary physical activity results in symptoms of HF. What stage of NYHA functional Classification?
Stage C | |
Stage D
| |
Class III
| |
Class IV |
Question 95 Explanation:
The guidelines state that class III is defined as an individual who has marked limitation of physical activity, comfortable at rest, but ordinary physical activity results in symptoms of HF. Class IV is defined as an individual who is unable to carry on any physical activity without symptoms of HF, or symptoms of HF at rest. Stage D is when an individual has refractory HF that requires specialized interventions. And Stage C is when there is structural heart disease with prior or current symptoms of HF.
Reference:
Yancy CW, Jessup M, Bozkurt B, et al. 2013 ACCF/AHA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines.J Am Coll Cardiol. 2013;62(16):e147-e239. doi:10.1016/j.jacc.2013.05.019. Retirved on Feb 6th from : http://circ.ahajournals.org/content/128/16/e240
Reference:
Yancy CW, Jessup M, Bozkurt B, et al. 2013 ACCF/AHA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines.J Am Coll Cardiol. 2013;62(16):e147-e239. doi:10.1016/j.jacc.2013.05.019. Retirved on Feb 6th from : http://circ.ahajournals.org/content/128/16/e240
Question 96 |
Which of the following medications are known to prevent heart failure in patients with myocardial infarction (MI)?
Statin
| |
Angiotensin-converting enzyme (ACE) Inhibitor or angiotensin-receptor blocker (ARB)
| |
Evidence-based beta blocker example bisoprolol, metoprolol succinate and carvedilol
| |
All of the above are known to prevent heart failure in patient with MI |
Question 96 Explanation:
All of the above are known to prevent heart failure in patients with MI. The guidelines state that in all patients with a recent or remote history of MI or ACS, statins should be used to prevent symptomatic HF and cardiovascular events. Those with known atherosclerotic disease are more likely to develop HF. Therefore, aggressive treatment with statins can help to reduce the likelihood of HF in at-risk patients. The guidelines also state that in all patients with a recent or remote history of MI or ACS and reduced EF, ACE inhibitors should be used to prevent symptomatic HF and reduce mortality. ARBs would be appropriate if patients are intolerant to ACE inhibitors. This can also be applied to beta-blockers. Patients with a recent or remote history of MI or ACS and reduced EF should use evidence-based beta-blockers to reduce mortality. In addition, ACE inhibitors and beta-blockers should be used in all patients with a reduced EF to prevent symptomatic HF, even if they do not have a history of MI.
Reference:
Yancy CW, Jessup M, Bozkurt B, et al. 2013 ACCF/AHA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines.J Am Coll Cardiol. 2013;62(16):e147-e239. doi:10.1016/j.jacc.2013.05.019. Retirved on Feb 6th from : http://circ.ahajournals.org/content/128/16/e240
Reference:
Yancy CW, Jessup M, Bozkurt B, et al. 2013 ACCF/AHA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines.J Am Coll Cardiol. 2013;62(16):e147-e239. doi:10.1016/j.jacc.2013.05.019. Retirved on Feb 6th from : http://circ.ahajournals.org/content/128/16/e240
Question 97 |
You are told by a patient that she takes a medication that is on AGS 2015 Beers Criteria, she seeks your advice on what she should do. Which of the following would be the most appropriate thing to say to your patient?
Continue taking the medication, medications on the Beers Criteria are potentially inappropriate medication not definitely inappropriate medication.
| |
Continue taking the medication for now and ask your clinician before stopping the medication if there is safer alternative.
| |
Stop taking the medication immediately since it’s on the Beers Criteria.
| |
Stop taking the medication and discuss with the clinician if there is a safer alternative. |
Question 97 Explanation:
The AGS 2015 Beers Criteria is a guide but should not replace clinical judgement. If the patient has been taking a medication and does not experience any adverse effects while also having their condition under control, then the medication will most likely be fine for the time being. There may be another alternative for the medication that could be safer but that would have to be discussed with their clinician. It will be a process to switch medications and the patient and clinician will have to work together through the process in order to have a successful transition to the new medication.
Reference:
I. Hanlon, Joseph T., Todd P. Semla, and Kenneth E. Schmader. "Alternative Medications for Medications in the Use of High‐Risk Medications in the Elderly and Potentially Harmful Drug–Disease Interactions in the Elderly Quality Measures." Journal of the American Geriatrics Society 63.12 (2015): e8-e18. II. Radcliff, Sue, et al. "American Geriatrics Society 2015 updated beers criteria for potentially inappropriate medication use in older adults." JOURNAL OF THE AMERICAN GERIATRICS SOCIETY 63.11 (2015): 2227-2246. Available at: http://onlinelibrary.wiley.com/doi/10.1111/jgs.13702/full
Reference:
I. Hanlon, Joseph T., Todd P. Semla, and Kenneth E. Schmader. "Alternative Medications for Medications in the Use of High‐Risk Medications in the Elderly and Potentially Harmful Drug–Disease Interactions in the Elderly Quality Measures." Journal of the American Geriatrics Society 63.12 (2015): e8-e18. II. Radcliff, Sue, et al. "American Geriatrics Society 2015 updated beers criteria for potentially inappropriate medication use in older adults." JOURNAL OF THE AMERICAN GERIATRICS SOCIETY 63.11 (2015): 2227-2246. Available at: http://onlinelibrary.wiley.com/doi/10.1111/jgs.13702/full
Question 98 |
Which of the following is a dichotomous variable?
Sex
| |
Pain yes/ Pain no
| |
alive / dead
| |
A, B and C. |
Question 98 Explanation:
Dichotomous data is considered categorical data that only has two categories, or two answer choices. All 3 answer choices have only 2 categories: sex has male or female, pain is yes or no, and alive or dead is only two options also.
Reference:
"Statistics at Square One | The BMJ". Bmj.com. 2016. Web. 7 Nov. 2016. Available at: http://www.bmj.com/about-bmj/resources-readers/publications/statistics-square-one
Reference:
"Statistics at Square One | The BMJ". Bmj.com. 2016. Web. 7 Nov. 2016. Available at: http://www.bmj.com/about-bmj/resources-readers/publications/statistics-square-one
Question 99 |
JM is a 78 YOW with a creatinine clearance of 24 mls/hr. According to the AGS 2015 Updated Beers Criteria for Potentially Inappropriate Medication Use in Older Adults which of the following medications should JM avoid due to an increased risk of bleeding?
Apixaban
| |
Dabigatran
| |
Fondaparinux
| |
All of the |
Question 99 Explanation:
In Table 6, the AGS recommends these medications be avoided in the case of a CrCl less than 30, though for apixaban it is less than 25. These medications can put the patient at risk for bleeding. Enoxaparin can be used in patients with a CrCl less than 30 but it is recommended to reduce the dose. Both Edoxaban and Rivaroxaban can be used in patients with a CrCl between 30 to 50 but their doses should be reduced as well.
Reference:
Radcliff, Sue, et al. "American Geriatrics Society 2015 updated beers criteria for potentially inappropriate medication use in older adults." JOURNAL OF THE AMERICAN GERIATRICS SOCIETY 63.11 (2015): 2227-2246. Available at: http://onlinelibrary.wiley.com/doi/10.1111/jgs.13702/full
Reference:
Radcliff, Sue, et al. "American Geriatrics Society 2015 updated beers criteria for potentially inappropriate medication use in older adults." JOURNAL OF THE AMERICAN GERIATRICS SOCIETY 63.11 (2015): 2227-2246. Available at: http://onlinelibrary.wiley.com/doi/10.1111/jgs.13702/full
Question 100 |
LM is a 66 years old male with a new diagnosis of diabetes. His past medical history includes hypertension for which he takes amlodipine 5mg daily and hydrochlorothiazide25mg daily. His cholesterol panel includes total cholesterol (TC) 222 mg/dL, low-density lipoprotein cholesterol (LDL-C) 105 mg/dL, triglycerides (TG) 330 mg/dL, and high-density lipoprotein cholesterol (HDL-C) 51 mg/dL. His vital signs include BP 125/75 mm Hg and HR 70 beats/minute. His physician put him on metformin 500mg by mouth twice daily. Besides metformin what is the other pharmacologic regimen that should be started on LM?
Atorvastatin 80mg daily
| |
Rosuvastatin 10mg daily
| |
Gemfibrozil 600mg twice daily
| |
Simvastatin 40mg daily |
Question 100 Explanation:
This patients has diabetes, is aged between 40 and 75 years, and has an LDL between 70 and 189 mg/dL , which places him in one of the four statin benefit groups. These characteristics also warrant using the Pooled Cohort Risk Assessment Equation to estimate his 10-year ASCVD risk. Using the ASCVD Risk Estimator, and assuming he is a nonsmoker and is Caucasian, his 10-year ASCVD risk is 22.1%. Since it is greater than 7.5%, he should receive a high intensity statin therapy. Rosuvastatin 10 mg and Simvastatin 40 mg are considered moderate-intensity statin therapies, and gemfibrozil is not a statin. A is the best option because Atorvastatin 80 mg is high intensity statin therapy.
Reference:
Stone N, Robinson J, Lichtenstein A et al. 2013 ACC/AHA Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults. Circulation. 2013;129(25 suppl 2):S1-S45. doi:10.1161/01.cir.0000437738.63853.7a. Retrieved on Feb 6th 2017 from : http://circ.ahajournals.org/content/129/25_suppl_2/S1
ASCVD Risk Estimator. Tools.acc.org. 2016. Available at: http://tools.acc.org/ASCVD-Risk-Estimator/ . Accessed June 8, 2016.
Reference:
Stone N, Robinson J, Lichtenstein A et al. 2013 ACC/AHA Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults. Circulation. 2013;129(25 suppl 2):S1-S45. doi:10.1161/01.cir.0000437738.63853.7a. Retrieved on Feb 6th 2017 from : http://circ.ahajournals.org/content/129/25_suppl_2/S1
ASCVD Risk Estimator. Tools.acc.org. 2016. Available at: http://tools.acc.org/ASCVD-Risk-Estimator/ . Accessed June 8, 2016.
Once you are finished, click the button below. Any items you have not completed will be marked incorrect.
There are 100 questions to complete.
|
List |

Comments are closed.